It is 487 days since the index case, or patient zero of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), emerged in Wuhan, China, on December 1st, 2019. To date, the virus has spread globally, infecting over 138 million individuals and claiming the lives of over 2.97 million.
Over 78 million people have recovered, however, many patients report the persistence of some symptoms of SARS-CoV-2 infection, including cough, insomnia, headaches, and body pains.
In a new study, appearing on the pre-print server medRxiv*, researchers at the University of Trieste and Istituto Auxologico Italiano IRCCS in Italy report that more than half of patients with previous mild-to-moderate symptomatic COVID-19 complained of the persistence of at least one symptom 12-months after the onset of the illness.
Persistent symptoms
SARS-CoV-2 can spread via respiratory droplets or aerosols and can cause a wide range of symptoms.
The most common symptoms include fever, cough, sore throat, loss of smell and taste, headache, body pains, and breathing difficulty. Though most of the infected individuals develop mild to moderate symptoms, some may experience severe disease.
As the pandemic evolves, clinicians observed that some symptoms might persist for a long time in a proportion of patients recovered from the infection’s acute phase. Persistent symptoms may take a toll on the lives of “long haulers,” the term used to describe patients who experience COVID-19 symptoms even after recovery. The condition is also known as chronic COVID, chronic COVID syndrome, and long COVID.
An increasing number of studies have focused on long COVID, but these primarily look at previously hospitalized severe COVID-19 patients, who reported symptoms up to six months after infection. The current study, however, aimed to evaluate the prevalence of COVID-19-related symptoms one year after the onset of mild to moderate disease.
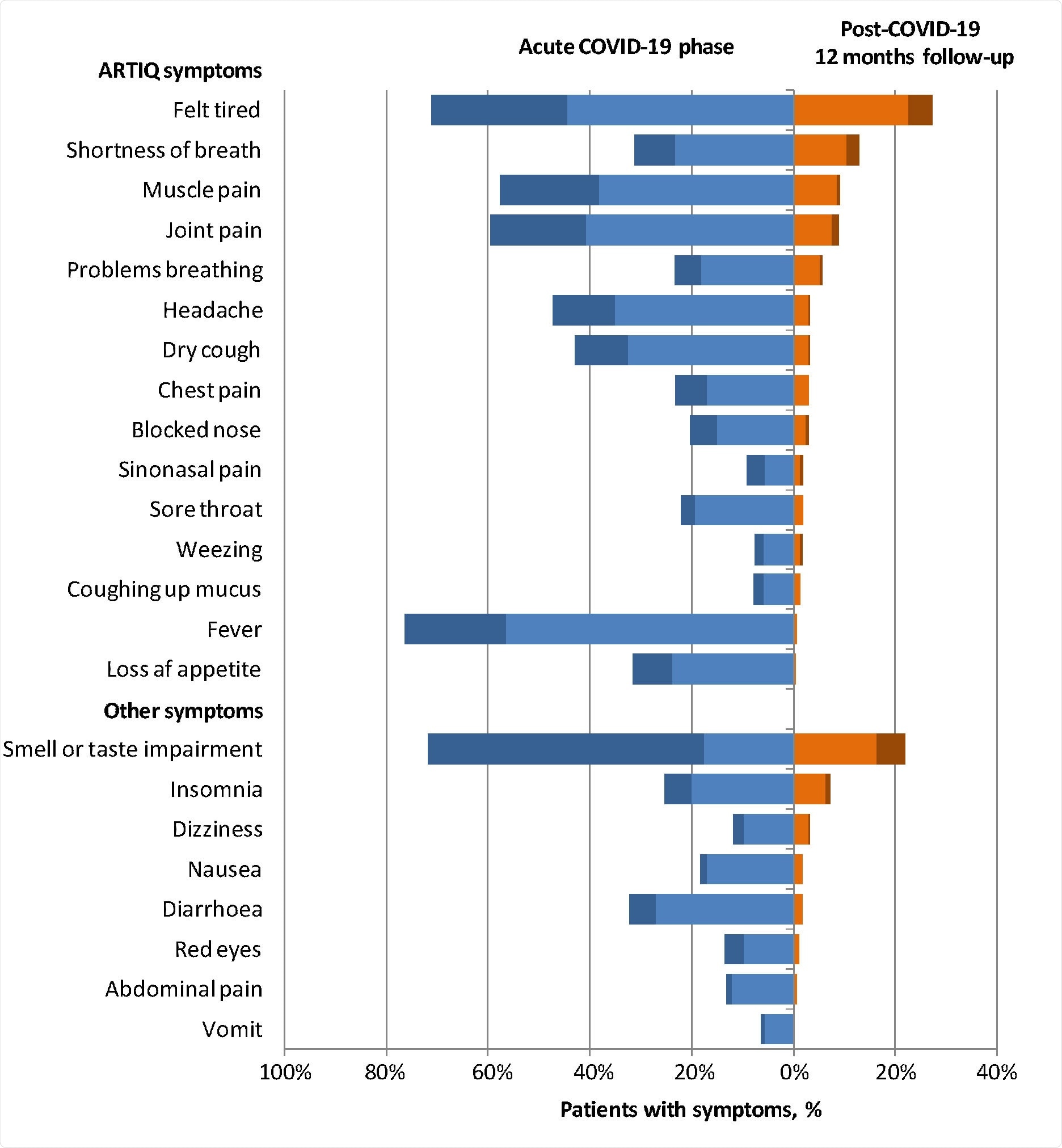
The figure reports the percentages of patients with COVID-19-related symptoms during the acute phase of illness (blue) and at 12-months follow-up (orange) according to severity (light=mild; dark=severe)
Long COVID in mild to moderate patients
To arrive at the study findings, the researchers conducted a prospective study on mild to moderate symptomatic adult patients consecutively assessed at Cattinara University Hospital, Trieste, Italy, from March 1 to March 31, 2020, who tested positive for SARS-CoV-2 RNA by polymerase chain reaction (PCR).
Initially, all patients were home-isolated with mild to moderate symptoms. The patients are considered to have mild symptoms if they have less severe clinical symptoms with no evidence of pneumonia. These patients do not require hospitalization.
Of the 304 patients completing the survey at baseline and follow-up interview, 161 or 53 percent of patients reported persistence of at least one symptom at 12 months follow-up. The most commonly reported symptom was fatigue or feeling tired, followed by an impaired sense of smell and taste, difficulty breathing or shortness of breath, and muscle pain.
Females, 40 to 54 years olds, those with a body mass index (BMI) higher than 30, and those who had more symptoms during the acute infection phase were more likely to experience long COVID.
People with long COVID may experience a significant impact on their quality of life and depression scale scores. The quality of life was markedly affected by fatigue, shortness of breath, and insomnia. Meanwhile, fatigue significantly impacted the depression scale.
The researchers conclude, “our study indicates that persistent symptoms of SARS-CoV-2 infection can be detected beyond 12- months from the onset of the illness in more than half of patients with mild-to-moderate disease. Identifying patients at risk for prevention and treatment will be critical to improving outcomes and reducing health costs. Finally, a structured and validated questionnaire for the assessment of symptoms in COVID-19 patients is highly desirable to characterize the full clinical spectrum of long COVID and improve the reliability and reproducibility of clinical studies.”
Source:
Journal reference: