Global rollout of vaccines to prevent coronavirus disease 2019 (COVID-19) is underway, with nine different vaccines approved for distribution by different countries. With four vaccines approved for distribution in the U.S., as of April 30, 2021, 29.9% of the U.S. population has now been fully vaccinated against SARS-CoV-2.
However, even with ongoing vaccination programs, reports indicate an increase in COVID-19 cases in some U.S. states. Despite these increases case numbers, several U.S. states have recently rescinded policies that make nonpharmaceutical interventions mandatory in public spaces and do not seem to have any intention of reinstating the measures.

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Epidemiological models of the effects of vaccine rollout on the transmission of SARS-CoV-2 indicate that the discontinuation of nonpharmaceutical interventions in the initial phases of vaccine rollout results in a subsequent spike in COVID-19 cases and leads to hospitalizations and deaths.
There are growing concerns that individuals will begin to shun nonpharmaceutical measures to prevent SARS-CoV-2 transmission and try to return to pre-pandemic normalcy before vaccine coverage levels can effectively minimize transmission risk.
Recent modeling in the U.S. shows that repealing nonpharmaceutical interventions too early will cause localized increases in the number of COVID-19 cases. However, the impact of nonpharmaceutical interventions on individual-level risk of SARS-CoV-2 infection in partially- and fully vaccinated populations is unclear.
Using an agent-based model to simulate SARS-CoV-2 transmission during indoor gatherings
Researchers from the U.S. recently used a previously published agent-based model (ABM) to simulate SARS-CoV-2 transmission in indoor settings, including gatherings of different population densities, durations, and vaccination status. The study is published on the preprint server, medRxiv*.
The study assumed that infectious individuals at indoor gatherings would be asymptomatic because people with symptoms would consciously stay away from these kinds of gatherings and that individuals with partial immunity were not part of the attendees of the gatherings.
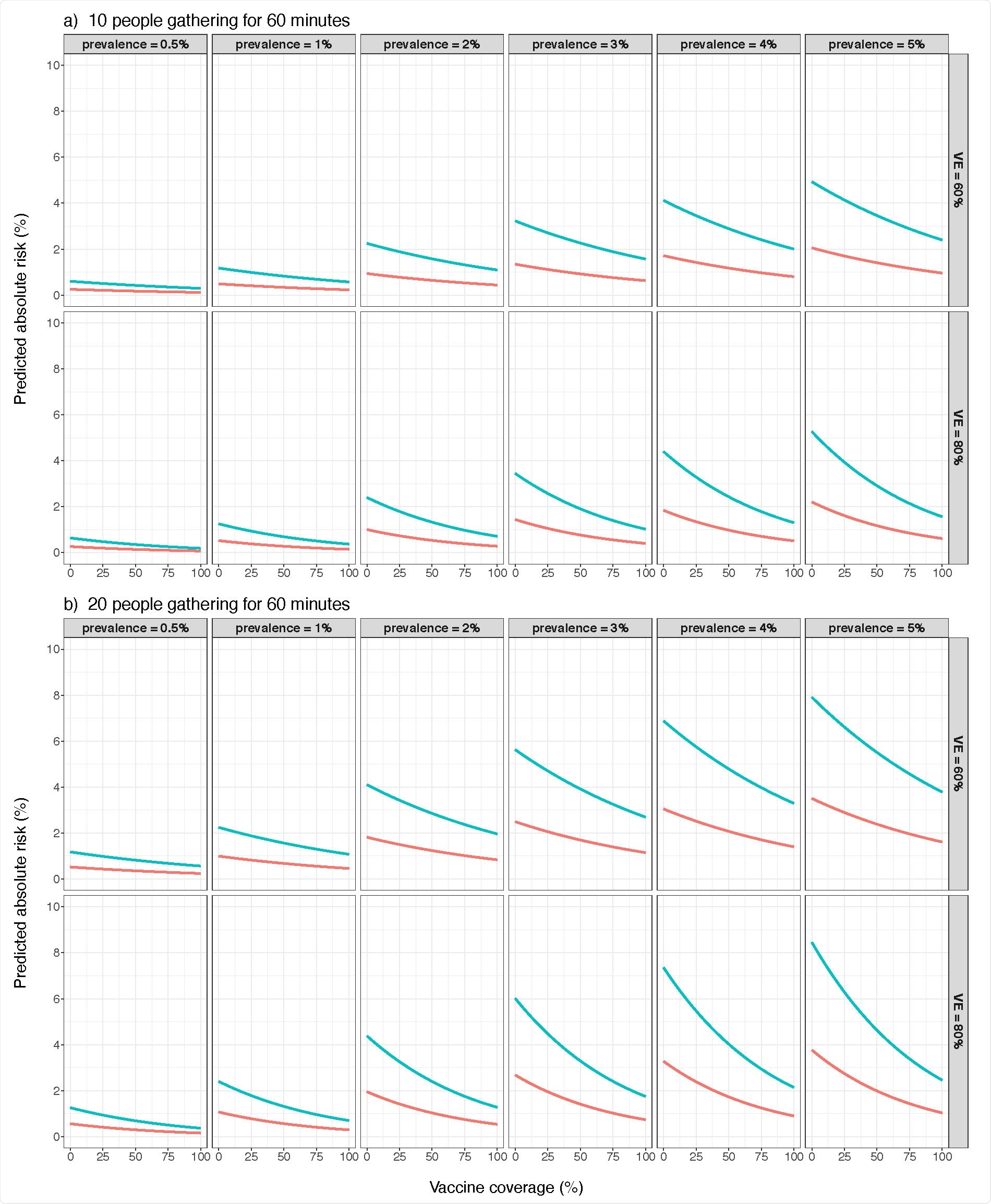
At low population densities and gathering duration limits, nonpharmaceutical interventions to prevent infection and elevated vaccination rates consistently decrease the probability of observing ≥ 1 successful SARS-CoV-2 transmission events in simulations.
Results show no definitive level of vaccination coverage that makes nonpharmaceutical interventions redundant
Using the ABM model, the researchers were able to quantify the difference in risk of SARS-CoV-2 infection in the presence and absence of nonpharmaceutical interventions.
“We previously used this model to quantify effects of nonpharmaceutical interventions on reducing SARS-CoV-2 transmission risk during an indoor superspreading event”
They found that nonpharmaceutical prevention measures often decrease secondary attack rates, especially in the case of brief interactions. Hence, there is no definitive level of vaccination coverage that makes nonpharmaceutical prevention strategies redundant.
However, they also found that the reduction of SARS-CoV-2 infection risk offered by nonpharmaceutical interventions could be proportional to the prevalence of COVID-19. If COVID-19 prevalence decreases in the U.S., nonpharmaceutical interventions may still offer protective effects, but the potential benefits of the interventions may be small enough to be considered “effectively negligible.”
“It is clear that at low population densities, 2-m social distancing confers additional protective effects when used in conjunction with cloth face coverings, even during relatively-long duration gatherings.”
Results may not reflect real-world situations as the study is based on simulated situations and behaviors
The authors warn that the study results must be viewed in the context of simulated situations and behaviors and may not be an exact reflection of the circumstances that exist in real-world transmission events. They added that although this is quite common in ABM-based studies, they believe that their model is accurate enough to highlight general trends in SARS-CoV-2 transmission and infection risk in indoor settings.
To summarize, the findings of this study indicate that nonpharmaceutical interventions are capable of reducing secondary attack rates, mainly during brief interactions. Hence there is no definitive vaccination coverage level that can potentially make nonpharmaceutical interventions fully redundant. Moreover, the beneficial effect of these interventions on reducing SARS-CoV-2 infection in the case of indoor gatherings may be dependent on COVID-19 prevalence.
“If U.S. COVID-19 prevalence decreases in the future, nonpharmaceutical interventions will likely still confer protective effects, but any potential benefits may be small enough to remain within “effectively negligible” risk thresholds.”

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.