There is a high fatality rate among the elderly following infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), with symptomatic coronavirus disease 2019 (COVID-19). As a result, elderly individuals, particularly those living in nursing homes, are highly vulnerable to being exposed to and experiencing the severe symptoms of COVID-19.
 Study: Infection fatality rate of COVID-19 in community-dwelling populations with emphasis on the elderly: An overview. Image Credit: sasirin pamai
Study: Infection fatality rate of COVID-19 in community-dwelling populations with emphasis on the elderly: An overview. Image Credit: sasirin pamai

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Background
Several early studies on COVID-19 were based on different cohorts of elderly people, with varying rates of underlying illness and different age groups. In particular, nursing home residents made up to 70% of fatalities due to COVID-19 in high-income countries during the first wave of the pandemic. The rapid rate at which this population was succumbing to COVID-19 was particularly striking, as the elderly generally comprise less than a hundredth of the populations in these countries.
The IFR in this subset has been thought to be as high as 25%, thus unduly boosting the community IFR. Moreover, statistics from this group have fluctuated wildly across countries due to differences in data collection and reporting. Thirdly, community-based seroprevalence studies typically do not include this group.
How was the study done?
In the current study, the researchers estimated the IFR in a community using data from multiple studies where the seroprevalence included the elderly. The primary aim was to define the IFR among the elderly.
Notably, the authors excluded seroprevalence studies based on healthcare workers, which might result in an above-average rate due to higher-than-usual exposure risk. Race and ethnicity records were also a precondition since both affect participation in such a study and the odds of acquiring COVID-19.
What did the study show?
In middle-income countries, the researchers found that a median of 53% of the location’s total COVID-19 deaths happened among the elderly. Comparably, in high-income countries, the elderly accounted for up to 86% of the location’s total COVID-19 deaths. When this same data point was refined to look at deaths that occurred in nursing home residents, a median of 44% occurred in middle-income countries.
Remarkably, the elderly comprised 9% and 15% of the population in middle-income and high-income countries, respectively. Furthermore, the percentage of people residing in nursing homes were between 0.08-0.20% and a median of 4.7% in middle-income and high-income countries, respectively.
In 14 countries, which consisted of 12 high-income and two middle-income countries, the IFRs of the elderly dwelling in the community were 2.4%. The IFR in the elderly was consistently higher in richer countries than in middle-income countries, at approximately 3% and 0.3%, respectively.
When individuals over the age of 85 were studied, the IFR steeply increased. For example, when people over the age of 85 accounted for 5% of the population, their IFR value was estimated to be around 0.62%. Comparably, when people over the age of 85 accounted for 10% and 20% of the population, the IFR rose to 1.18% and 4.29%, respectively.
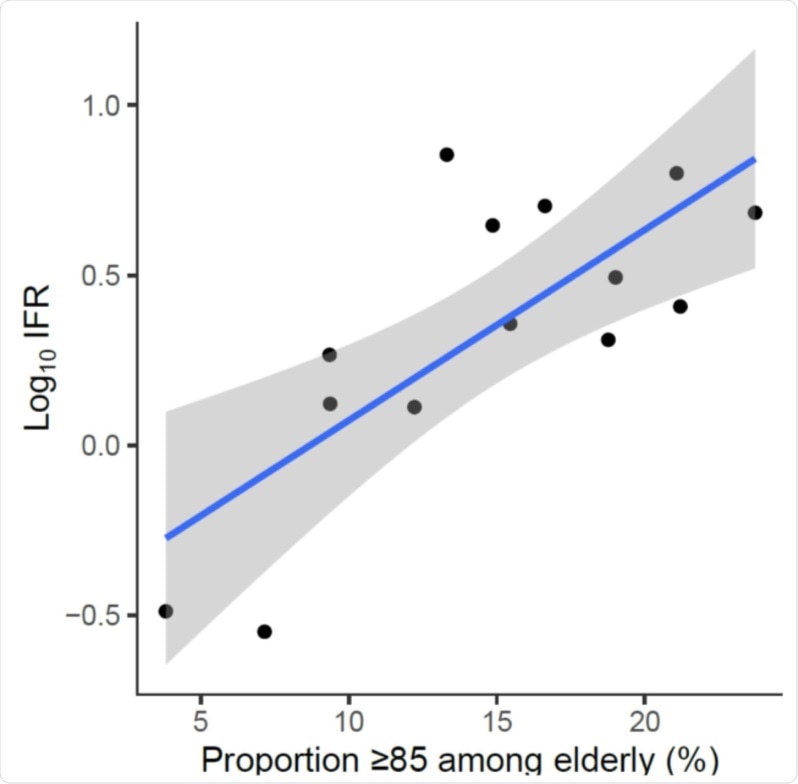 Infection fatality rate, corrected for unmeasured antibody types, plotted against the proportion of people ≥85 years old among the elderly. Log10 IFR: logarithm (with base 10) of the infection fatality rate. The “elderly” group is defined by the primary cutoff for each location. E.g. for Belgium 3% of the population is ≥85, and 13.6% of the population is ≥70, thus the proportion is 3/13.6. Imputation done for regional data: Denmark (3/5 regions), and Tamil Nadu, India, with country-level proportion of persons ≥85 years old among elderly.
Infection fatality rate, corrected for unmeasured antibody types, plotted against the proportion of people ≥85 years old among the elderly. Log10 IFR: logarithm (with base 10) of the infection fatality rate. The “elderly” group is defined by the primary cutoff for each location. E.g. for Belgium 3% of the population is ≥85, and 13.6% of the population is ≥70, thus the proportion is 3/13.6. Imputation done for regional data: Denmark (3/5 regions), and Tamil Nadu, India, with country-level proportion of persons ≥85 years old among elderly.
Low IFRs among the younger age groups
When studying IFR in individuals between the ages of 0 and 19 years, the researchers found that, across all countries, the median IFR was 0.0027%. The median IFR also remained low at 0.014% when individuals between the age of 20 and 29 were studied.
However, as the age groups started to increase, their IFR values followed. For example, individuals between the ages of 30-39 and 40-49 had IFR values of 0.031% and 0.082%, respectively. Even as older adults between the ages of 50 and 69 were studied, their IFR values also rose but remained under 1%.
Taken together, the findings of the current study indicate that location is a major determinant of IFR among the elderly. Secondly, nursing home residents have a dramatically higher IFR specific to COVID-19 as compared to the elderly who are living in the community. Since the use of assisted-care facilities is much more pronounced in high-income countries, this difference is brought out in this review.
Comparison with earlier research
Earlier data on age-specific IFR estimates used seroprevalence data along with COVID-19-related mortality data stratified by age. Some researchers have suggested IFRs of approximately 5% and 15% at age 75 and 85, respectively. However, these estimates did not include nursing home deaths and were based on limited data in the elderly age groups.
These studies also came from locations with a high incidence rate and used a very long period within which deaths were counted as being due to COVID-19.
The Imperial College London also presented high IFRs among the elderly, mostly because they used very narrow selection criteria, including only 10 studies in nine countries, with half of them including more than a thousand subjects. Their selection bias was obvious since only hard-hit areas were included in the study.
The current study estimates lower IFRs, not only among the elderly, but also among those younger than 50 years. Among those aged <19 years and 30-39 years, the median IFR is <1/40,000, while in the age group 20-29 years, it is 1/71,000.
For those above 40, one in 1,200 are estimated to die from COVID-19. These estimates are inflated 5-10 times in the Imperial College study for those aged 0-29 years.
What are the implications?
Since both the current and earlier studies indicate a very low IFR in individuals between 30 and 50 years, this data is potentially important for evaluating the risk-benefit ratio of interventions such as vaccinations in these younger populations.
Further research will hopefully provide more information on the role of other factors besides age and being a nursing home resident. Obesity, for example, affects over a third of the people in high-income countries, but less than 5% in low- and middle-income countries. Other factors, such as smoking history, diabetes, and cardiovascular disease, all of which are associated with more severe COVID-19 symptoms, are also more common in high-income countries.
Finally, it is noteworthy that the IFR in nursing home residents dropped sharply after the first wave due to the use of better evidence-based guidelines.
Overall, the IFR was much lower in community-based elderly people than estimated for the elderly population overall. The difference in IFRs is greatest when nursing home care is much more common as a form of care for the elderly. However, IFRs were lower among the middle-aged.
“The estimates presented here may serve as one of several key pieces of information underlying public health policy decisions. With better measures, in particular vaccines, hopefully IFR estimates have already decreased further.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources