Scientists across the globe have worked at record speed to develop vaccines against the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), which is the virus responsible for the coronavirus disease 2019 (COVID-19).
Several of these vaccines have received emergency use authorization (EUA) from numerous regulatory bodies, which has allowed for the initiation of vaccination programs in many countries around the world. One of the approved messenger ribonucleic acid (mRNA)-based vaccines is BNT162b2, which has been reported to be highly effective against symptomatic COVID-19 disease.
 Study: Long-term immunogenicity of BNT162b2 vaccination in the elderly and in younger health care workers. Image Credit: Yuganov Konstantin / Shutterstock.com
Study: Long-term immunogenicity of BNT162b2 vaccination in the elderly and in younger health care workers. Image Credit: Yuganov Konstantin / Shutterstock.com

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Background
Recent studies have revealed that vaccine-induced antibodies remained stable for about six months. To date, all of the vaccines that received EUA have been developed against the spike (S) protein of the original SARS-CoV-2 strain.
Owing to the ability of this virus to frequently mutate, several SARS-CoV-2 variants have emerged. These variants have been classified as either variants of interest (VoI) and variants of concern (VoC) according to their virulence and rate of transmission.
The emergence of SARS-CoV-2 variants, especially the Delta variant, has questioned the effectiveness of many vaccines. Scientists have revealed that vulnerable groups such as the elderly who have been vaccinated using the BNT162b2 vaccine are at a higher risk of contracting the SARS-CoV-2 Delta variant as compared to younger adults.
Many studies have reported a surge in the rate of COVID-19, especially due to the dominant circulating Delta strain, in highly vaccinated populations. These reports have prompted authorities in several countries, such as the United States, Israel, and Germany, to discuss the effectiveness of a third booster dose to vulnerable patient populations, such as those over the age of 60.
A new study
Since the sustenance of vaccine-induced immunity in the elderly is not clear, a new cohort study comparing immune responses among vaccinated elderly persons and healthcare workers (HCW) has been conducted. The authors of this study, which is available on the medRxiv* preprint server, determined the immune responses six months after the first vaccination with BNT162b2.
In this study, six months follow-up visits were completed for 107 HCW, whose median age was estimated to be 35 years, as well as 82 elderly persons whose median age was 82.5 years. In both the study groups, females were in majority.
The authors of this study excluded participants who contracted COVID-19, as confirmed by reverse-transcriptase polymerase chain reaction (RT-PCR), after receiving the first or second dose of the BNT162b2 vaccine.
Study findings
The current study revealed that the anti-SARS-CoV-2 S1-immunoglobulin G (IgG) seropositivity rates decreased in the elderly group as compared to the HCW group six months post-vaccination. The researchers also found that the lowering of anti-RBD- and anti-full S-IgG levels in the serums of the elderly group was more pronounced than HCWs. The current study also reports a significant decrease in surrogate virus neutralization (sVNT) titers among the elderly at 56% as compared to 88.1.
In the current study, the researchers used the pseudovirus neutralization test (pNT) to determine the neutralization of the Delta variant post-vaccination. They revealed a substantial decline of serum neutralization of the Delta variant two months after the subjects received the first dose of vaccine and four weeks after the second dose.
In 60.6% of the elderly vaccinated group, serum neutralization of the Delta variant was observed six months after vaccination. However, this was not the case in the younger study group containing HCWs, where 95.2% of the HCW cohort could neutralize the same variant six months post-vaccination.
This study also evaluated the neutralization of the Alpha variant in the same cohorts. To this end, 95.2% of HCWs and 69.0% of the elderly cohort could neutralize the Alpha variant six months following complete BNT162b2 vaccination. As expected, the mean neutralizing titers for both Alpha and Delta variants were significantly reduced in the elderly group as compared to younger HCWs.
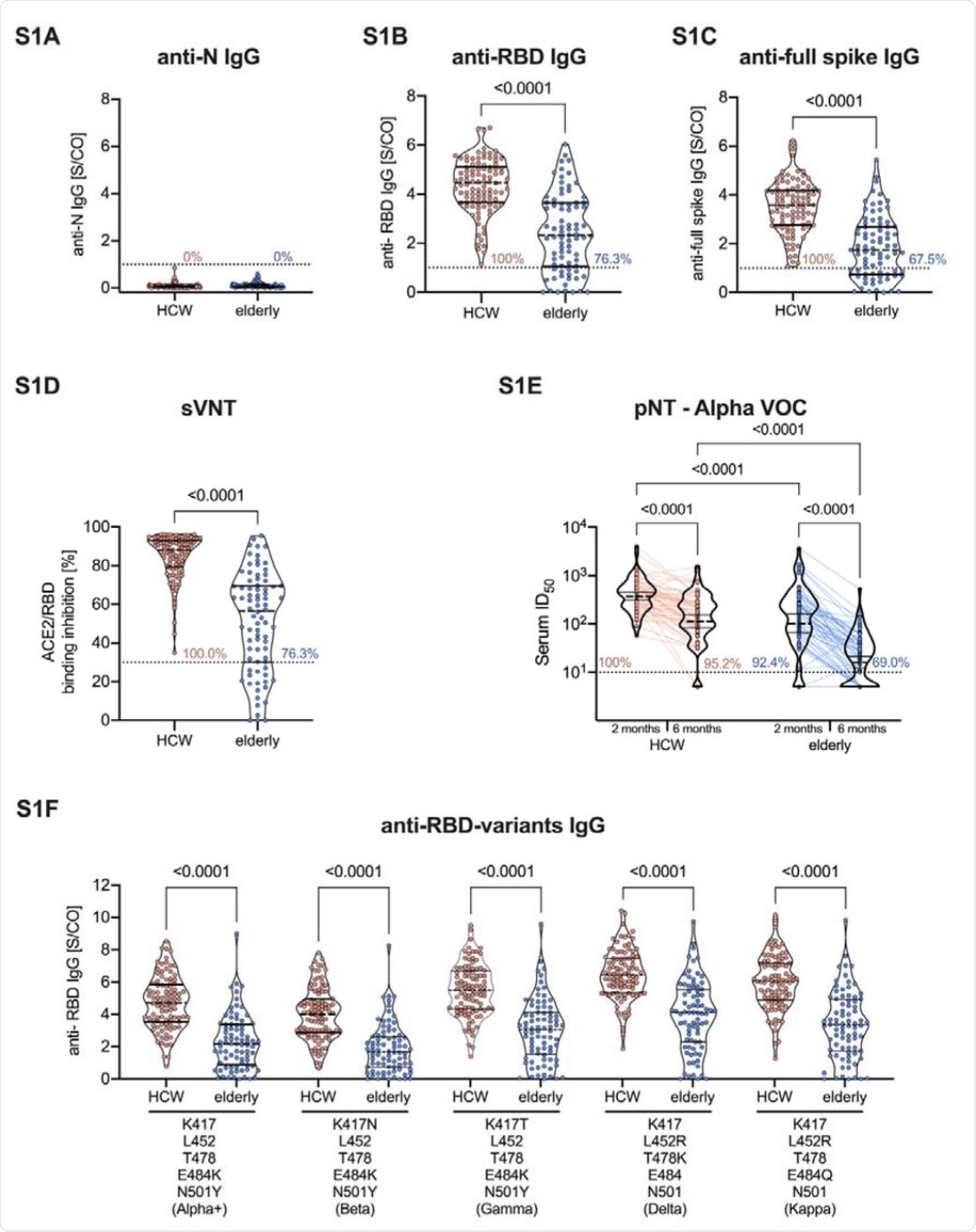 (A) Anti-SARS-CoV-2 N, (B) RBD- (C) and full-spike IgG measured in the serum of BNT162b2 vaccinated HCW and elderly persons six months after the first vaccination. (D) Neutralizing capacity was measured by sVNT and (E) serum neutralization against Alpha (B.1.1.7) VOC detected by pNT in vaccinated HCW and elderly persons six months after the first vaccination. (F) Binding capacity of serum IgG against six different RBDs of SARS-CoV-2 variants carrying the indicated mutations in HCW and elderly, measured by ELISA. Dotted lines indicate the manufacturer’s threshold values: for anti-N, anti-RBD, and anti-full spike IgG ≥1 S/Co, for sVNT >30%, and the lower limit of detection (1:10 dilution) for pNT. Lines indicate the median and interquartile range except for pNT, where the geometric mean and 95% confidence interval are shown. P values were calculated by the non-parametric Mann Whitney U test or Kruskal-Wallis test with Dunn’s multiple comparisons test. S/Co: signal-to-cutoff, N: nucleocapsid protein, RBD: receptor-binding domain, sVNT: surrogate virus neutralization test, ACE2: angiotensin-converting enzyme 2, ID50: 50% inhibition dilution.
(A) Anti-SARS-CoV-2 N, (B) RBD- (C) and full-spike IgG measured in the serum of BNT162b2 vaccinated HCW and elderly persons six months after the first vaccination. (D) Neutralizing capacity was measured by sVNT and (E) serum neutralization against Alpha (B.1.1.7) VOC detected by pNT in vaccinated HCW and elderly persons six months after the first vaccination. (F) Binding capacity of serum IgG against six different RBDs of SARS-CoV-2 variants carrying the indicated mutations in HCW and elderly, measured by ELISA. Dotted lines indicate the manufacturer’s threshold values: for anti-N, anti-RBD, and anti-full spike IgG ≥1 S/Co, for sVNT >30%, and the lower limit of detection (1:10 dilution) for pNT. Lines indicate the median and interquartile range except for pNT, where the geometric mean and 95% confidence interval are shown. P values were calculated by the non-parametric Mann Whitney U test or Kruskal-Wallis test with Dunn’s multiple comparisons test. S/Co: signal-to-cutoff, N: nucleocapsid protein, RBD: receptor-binding domain, sVNT: surrogate virus neutralization test, ACE2: angiotensin-converting enzyme 2, ID50: 50% inhibition dilution.
The scientists observed that the emergence of viral variants containing mutations like E484K, which cause evasion of vaccine-induced immune responses or immune responses due to natural COVID-19 infection, would further reduce immunity among the old age group.
In the elderly group, the researchers found a reduction in the binding capacity of serum antibodies to RBDs containing mutations such as K417N/T, L425R, T478K, E484K/Q, N501Y, and E484Q. These mutations are present in six known SARS-CoV-2 variants, thereby indicating that the vaccinated elderly group is still highly susceptible to COVID-19.
However, this reduction in binding capacity was not observed in the HCW cohort. The current research also revealed a reduction in the SARS-CoV-2-S1 T-cell reactivity in the elderly when compared to HCWs.
Conclusion
The authors of the current study indicated a significant waning of immune responses induced via COVID-19 vaccination in the elderly. However, neutralizing capacity was still detected after six months of initial vaccination in the younger group of HCWs.
This study showed a significant reduction in immunogenicity markers in the elderly six months post-vaccination. It also provided evidence that a two-dose vaccination regimen induces a less stable immune response in the elderly group as compared to younger groups.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Tober-Lau, P., Schwarz, T., Vanshylla, K., et al. (2021) Long-term immunogenicity of BNT162b2 vaccination in the elderly and in younger health care workers. medRxiv. doi:10.1101/2021.08.26.21262468. https://www.medrxiv.org/content/10.1101/2021.08.26.21262468v1.
- Peer reviewed and published scientific report.
Tober-Lau, Pinkus, Tatjana Schwarz, Kanika Vanshylla, David Hillus, Henning Gruell, Norbert Suttorp, Irmgard Landgraf, et al. 2021. “Long-Term Immunogenicity of BNT162b2 Vaccination in Older People and Younger Health-Care Workers.” The Lancet Respiratory Medicine 9 (11): e104–5. https://doi.org/10.1016/S2213-2600(21)00456-2. https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(21)00456-2/fulltext.