A modeling study led by Kuan-lin Huang of the Icahn School of Medicine at Mount Sinai in New York suggests that getting vaccinated and taking preventative measures such as social distancing and mask-wearing is the most effective way to curb the spread of severe acute respiratory coronavirus 2 (SARS-CoV-2). Their preprint medRxiv* study estimates that the trajectory of the pandemic will largely depend on the level of natural and vaccine-induced immunity in the area.
By September 2021, over half of the American population will be fully vaccinated. SARS-CoV-2 variants, such as the Delta variant dominant in the United States, have genetic mutations that make them more contagious and are more likely to cause severe infection in unvaccinated people.
How they did it
A mathematical model was designed that estimated the spread of SARS-CoV-2 in the United States. Factors such as vaccination rates, vaccine effectiveness, and waning immunity after six months influenced estimates.
The vaccine-induced immunity was based on receiving one or two doses of the Pfizer-BioNTech vaccine against the Delta variant. They projected about 45% of the U.S. population would have one vaccine dose, and 40% would have two doses by August 2021. Therefore, by October 2021, they assumed a 60% vaccination rate for one dose and approximately 50% for two doses.
The researchers also included parameters from data on daily infections and deaths from the John Hopkins University coronavirus database.
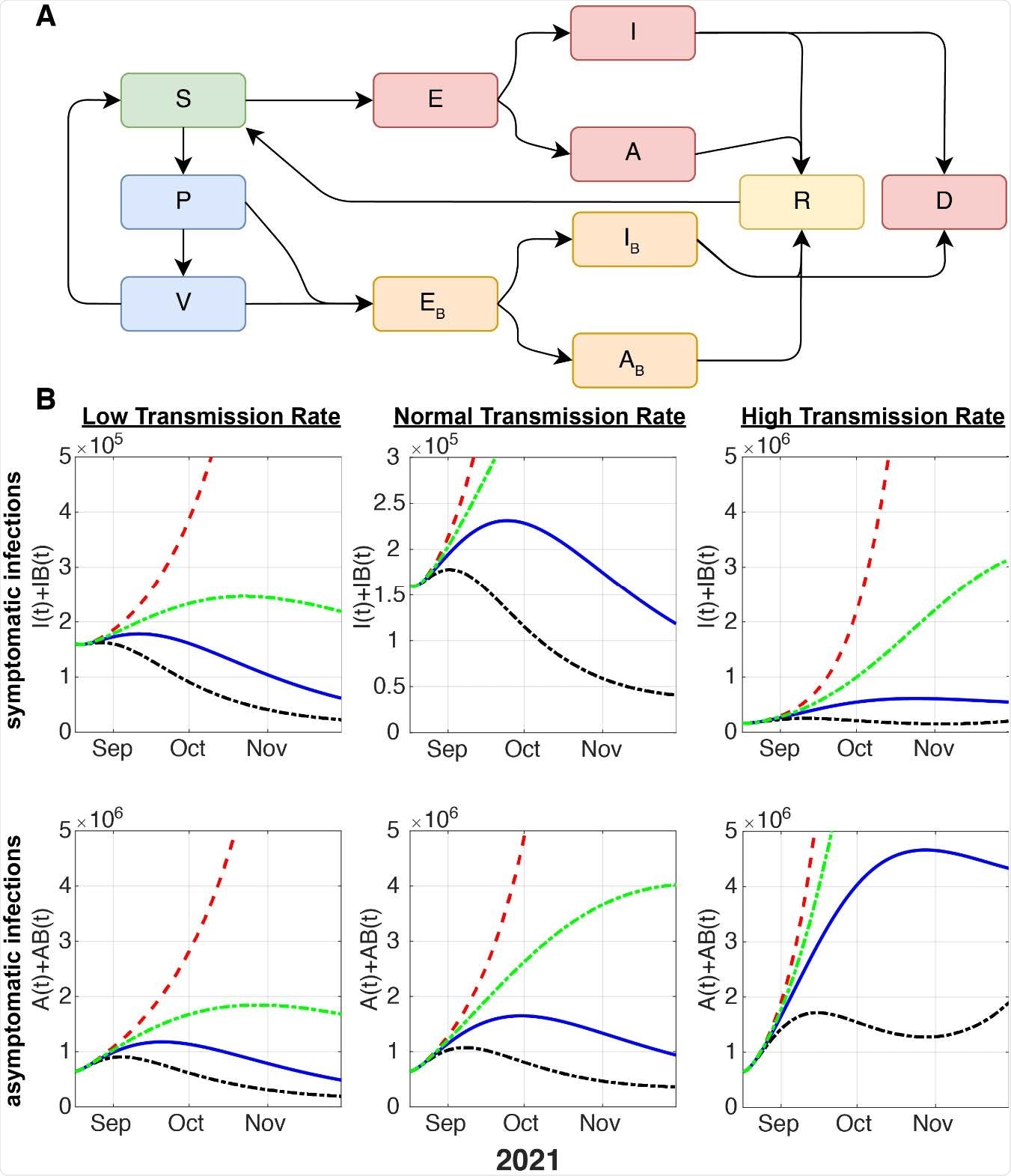
Schematic of the model considering vaccinated vs. unvaccinated individuals and projection of newly infected symptomatic and asymptomatic cases. (A) Flow dynamics of the mathematical model. S: susceptible, P: partial immunity (one vaccine dose), V: full immunity (two vaccine doses). E: unvaccinated, exposed. I: unvaccinated, infected and symptomatic, A: unvaccinated, infected, asymptomatic. ����: vaccinated (≥1 ��������), exposed. ����: vaccinated (≥1 ��������), infected, and symptomatic (“breakthrough cases”). ����: vaccinated (≥1 ��������), infected and asymptomatic. R: recovered. D: deceased. (B) Modelled dynamics of the new infections that are symptomatic (top row) and asymptomatic (bottom row) from the SARS-CoV-2 delta variant considering different vaccination rates. The red line presents zero vaccination; the green line represents a 50% decrease in VR; the blue dotted line means baseline VR and the black dotted line denotes 200% VR.
Model estimates for controlling the pandemic
Regardless of the transmission rate, there would be an exponential increase in an entire unvaccinated population.
If the SARS-CoV-2 virus has a high transmission rate, new infections would be significantly higher, and a 200% vaccination rate would be needed to control the pandemic.
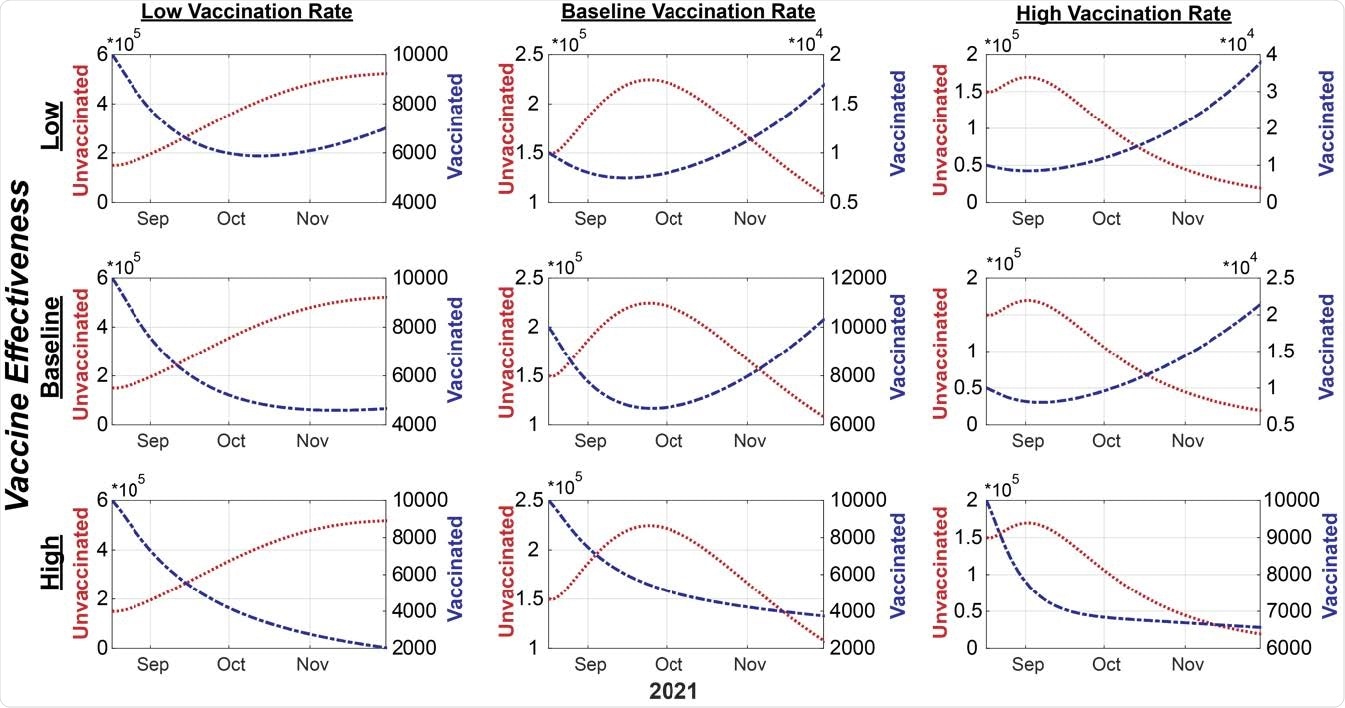
Modelled projections of symptomatic infections in unvaccinated and vaccinated subpopulations under different vaccination rates and vaccine effectiveness. The case counts of the unvaccinated individuals are depicted by the red line and the unit labels on the left-side y-axis, whereas the infected, vaccinated (breakthrough) cases are depicted by the blue line and the unit labels on the right-side y-axis.
Higher risk of infection in unvaccinated individuals
Vaccinated individuals have a lower risk of getting infected, though a small number of breakthrough Delta-related cases have been reported.
The models based their estimates on low versus high vaccine effectiveness. Low vaccine effectiveness was individuals with one dose, and high vaccine effectiveness was fully vaccinated individuals.
Even when vaccine effectiveness decreased in the face of Delta, the number of symptomatic COVID-19 infections was 10x magnitude higher in unvaccinated individuals than vaccinated individuals. At 50% vaccine uptake, new symptomatic infections are projected to continue rising in unvaccinated individuals.
Breakthrough infections in vaccinated individuals are more likely in a population with low vaccine uptake. “Notably, due to the higher number of individuals becoming vaccinated under baseline or 200% VR scenarios, new, symptomatic infections from vaccinated individuals (“breakthrough cases”) were projected to rise in October 2021 if the vaccine effectiveness is at low or baseline levels,” explained the team.
However, if vaccination rates increase, the number of breakthrough cases will decrease.
Vaccination rates would also impact the number of COVID-19 deaths. But, conversely, higher vaccination rates would help prevent deaths.
Additionally, if 30% of the population recovered from infection and gained natural immunity, about 67% will still need partial vaccination to reach herd immunity. Assuming low viral transmission, the model estimates that about 55% of the population will need partial vaccination to achieve herd immunity.
Overall, the researchers suggest vaccinating a majority of the population and practicing preventative COVID-19 measures is necessary to prevent further spread of the Delta variant.
Study limitations
The model did not consider the individual differences between the population in different communities and states. Therefore, depending on where a person lives, the number of vaccinated individuals may be smaller than what is required to achieve herd immunity — potentially increasing the risk for breakthrough infections.
The researchers did not consider how seasons influenced the spread of SARS-CoV-2. From the previous year, COVID-19 cases increased in the winter compared to the summer. A seasonality trend may impact the model’s estimates of cases.
Since Delta overtook Alpha as the most dominant SARS-CoV-2 strain, the research team predicted the number of future Delta-related infections. The model also based their predictions on how protective the Pfizer-BioNTech vaccine could be towards the Delta variant. Finally, the researchers assure that the model can be applied to other vaccines and other emerging SARS-CoV-2 strains.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources