Diverse coronavirus (CoV) strains can infect both animals and humans and bring about different diseases. CoVs are known to have caused three epidemics and pandemics in the last two decades. Therefore, knowledge on the evolution and emergence of CoV diversity in animals and humans is of importance.
Coronavirus disease 19 (COVID-19) was first identified in China in December 2019, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Later in March 2020, it was declared a global pandemic by the World Health Organization (WHO).
The four genera of coronavirus include the alpha-coronavirus (α-CoV), beta-coronavirus (β-CoV), gamma-coronavirus (γ-CoV), and delta coronavirus (δ-CoV). All of the four subtypes fall under the Orthocoronaviridae. The α- and β-CoV are known to infect mammals, γ-CoV infects avian species while δ-CoV infects both mammalian and avian species.
A study published in the Virus journal aimed to understand the evolutionary and epidemiology dynamics of coronavirus diversity in animals, humans, and wildlife at ecosystem interfaces.
The study
The study involved a detailed literature search using specific keywords in PubMed, Scopus, Google Scholar, and Web of Science on the natural infection of coronaviruses in humans, animals, and wildlife. Grey literature was also searched regarding the diversity of human and animal coronaviruses. The literature was selected based on their natural infection among different species. Furthermore, information regarding the number of cases and timeline of the emergence of different animal and human CoVs was also collected.
Several phylogenetic trees were prepared to determine the ancestral relationships between the human and animal coronaviruses. Several representative sequences of CoVs from humans, animals, and wildlife were aligned and finally assessed by phylogenetic analysis.
Study findings
Emerging and endemic CoVs infection in livestock and companion animals
A wide range of livestock CoVs produce different diseases in different domesticated animals, but not all of them have zoonotic potential. The bovine coronavirus (BCoV) has a wide range of hosts and is also genetically related to human β-CoV OC43. Besides BCoV, a critical pig coronavirus, swine acute diarrhea syndrome virus (SADS-CoV) can pose a serious threat to human health. However, the nucleotide similarity between porcine CoV and SARS-CoV-2 is low, suggesting that SARS-CoV-2 did not emerge from pigs.
A high similarity exists between the porcine angiotensin-converting enzyme 2 (ACE2) and human ACE2, which suggests that SARS-CoV-2 is capable of infecting pigs. Though pigs are not susceptible to SARS-CoV-2, cross-species transmission and mutation may occur with porcine CoV.
Emerging CoVs in wildlife
Bats are known to be the ancestors of SARS, MERS, SARS-CoV-2, and other significant CoVs that threaten human and animal health. Palm civets and raccoon dogs were found to be intermediate hosts of SARS-CoV-like viruses. Additionally, the civet strains of SARS-like CoVs were closely related to the human strains that led to the 2002-2003 SARS outbreak.
The results also indicated that several wild species infections of SARS-CoV-2 occurred from humans. These wild animal species may help in further evolution and transmission of CoV to other susceptible animals. For instance, the infection in minks was initiated by humans that led to the emergence of a new mink variant. This leads to the persistence of the virus in nature and its emergence from time to time.
The marine CoVs were found to be highly similar to the human coronaviruses. As a result of human infection, there is a high chance of SARS-CoV-2 being released in the marine environment. The nucleic acid of SARS-CoV-2 has been detected in wastewater and sewage water to transmit to wild aquatic animals.
Emerging and endemic CoVs infection in humans
The endemic human CoVs include OC43, 229E, NL63, and HKU1. All of them are animal-borne whose spillover events have already been proven. Three pandemic CoVs, SARS, MERS, and SARS-CoV-2, originated from animals, mostly Rhinolophus bats.
The ongoing pandemic, caused by the SARS-CoV-2, spread from a seafood and wild animal market in China. Initially, infection occurred from animal or environmental contacts leading to animal-to-human transmission, but recent studies have shown human-to-human transmission occurs through respiratory droplets. Hospital-acquired infection is also a major cause of SARS, MERS, and SARS-CoV-2 infection.
The structural analysis of SARS-CoV-2 showed that although they use the same receptor for entry like SARS-CoV, the affinity for the receptor is much higher in the case of SARS-CoV-2. This indicates that SARS-CoV-2 could be more infectious to humans as compared to SARS-CoV.
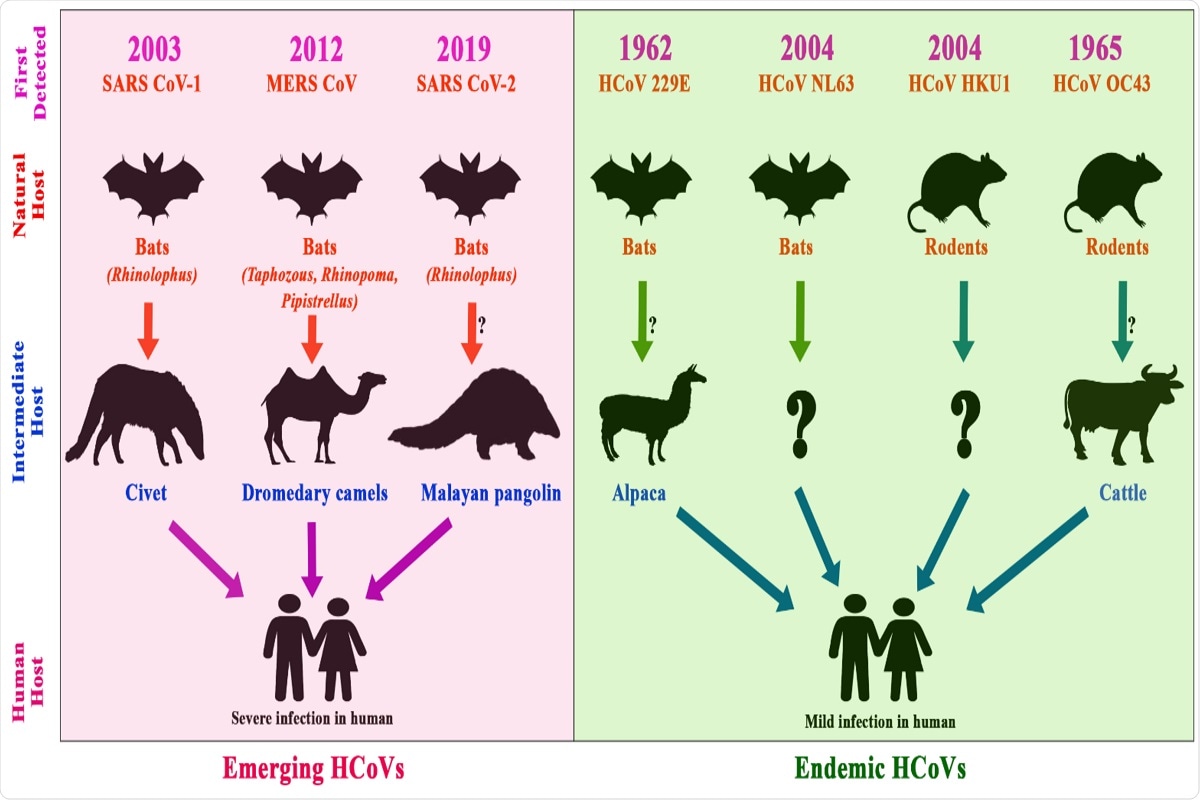 Figure 5. Timeline of the emergence of human CoVs, their reservoirs, and intermediate hosts; the pink shaded area depicts emerging coronaviruses, whereas the green shaded area depicts the endemic coronaviruses. The arrows show the transmission route of the viruses from animal to human through intermediate hosts.
Figure 5. Timeline of the emergence of human CoVs, their reservoirs, and intermediate hosts; the pink shaded area depicts emerging coronaviruses, whereas the green shaded area depicts the endemic coronaviruses. The arrows show the transmission route of the viruses from animal to human through intermediate hosts.
Conclusion
The current study showed that many animals, both wild and domesticated and humans, are susceptible to various CoVs. There is considerable evidence of cross-species transmission that leads to new strains and increased transmissibility of CoVs. The coronavirus strains causing the pandemics and endemics impacted public health, the global economy, and society. Strengthening animal surveillance could prevent the outbreak of CoVs from animal sources.