To this end, the researchers of the current study found that the hospitalization and mortality rates were significantly higher among rural patients. They also found similar observations of high mortality rates in rural persons without SARS-CoV-2 infection.
 Study: Higher hospitalization and mortality rates among SARS-CoV-2 infected Persons in Rural America. Image Credit: Jacob Haskew / Shutterstock.com
Study: Higher hospitalization and mortality rates among SARS-CoV-2 infected Persons in Rural America. Image Credit: Jacob Haskew / Shutterstock.com

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Background
SARS-CoV-2, which was first identified in late 2019 in Wuhan, China, causes coronavirus disease 2019 (COVID-19), with cough, fever, and respiratory distress. COVID-19 may be clinically mild or severe; however, it can also result in mortality.
Although the initial COVID-19 cases were largely in urban areas, by late 2020, rural communities also experienced high SARS-CoV-2 infection rates and soaring COVID-19 cases in the U.S.
The social, economic, and environmental factors are distinct between the rural and urban communities. Rural inhabitants, for example, are older, less likely to engage in behaviors to prevent SARS-CoV-2 infection and often exhibit a higher prevalence of comorbidities that are associated with severe COVID-19 and death.
With scarce resources in the rural areas, the impact of the COVID-19 pandemic in these areas is largely unknown. Coupled with limited data on COVID-19 in rural areas, which is rarely centralized, there is limited research on SARS-CoV-2 infected rural-urban discrepancies.
To understand the drivers of COVID-19 outcomes in rural America, the researchers assessed and compared COVID-19 related hospitalization and mortality rates in rural and urban areas.
About the study
To assess hospitalization rates and all-cause inpatient mortality among persons with definitive COVID-19 diagnoses residing in rural and urban areas, the researchers used the National COVID Cohort Collaborative (N3C), a National Institutes of Health-supported data enclave containing electronic health record information on people tested for SARS-CoV-2 and on patients diagnosed with SARS-CoV-2 infection.
This retrospective study from N3C examined a cohort of 573,018 patients, of whom 117,897 were hospitalized, from 27 U.S. hospital systems. These patients presented SARS-CoV-2 infection between January 2020 and March 2021.
The researchers also included a sample of 450,725 hospitalized persons without COVID-19 diagnoses for comparison.
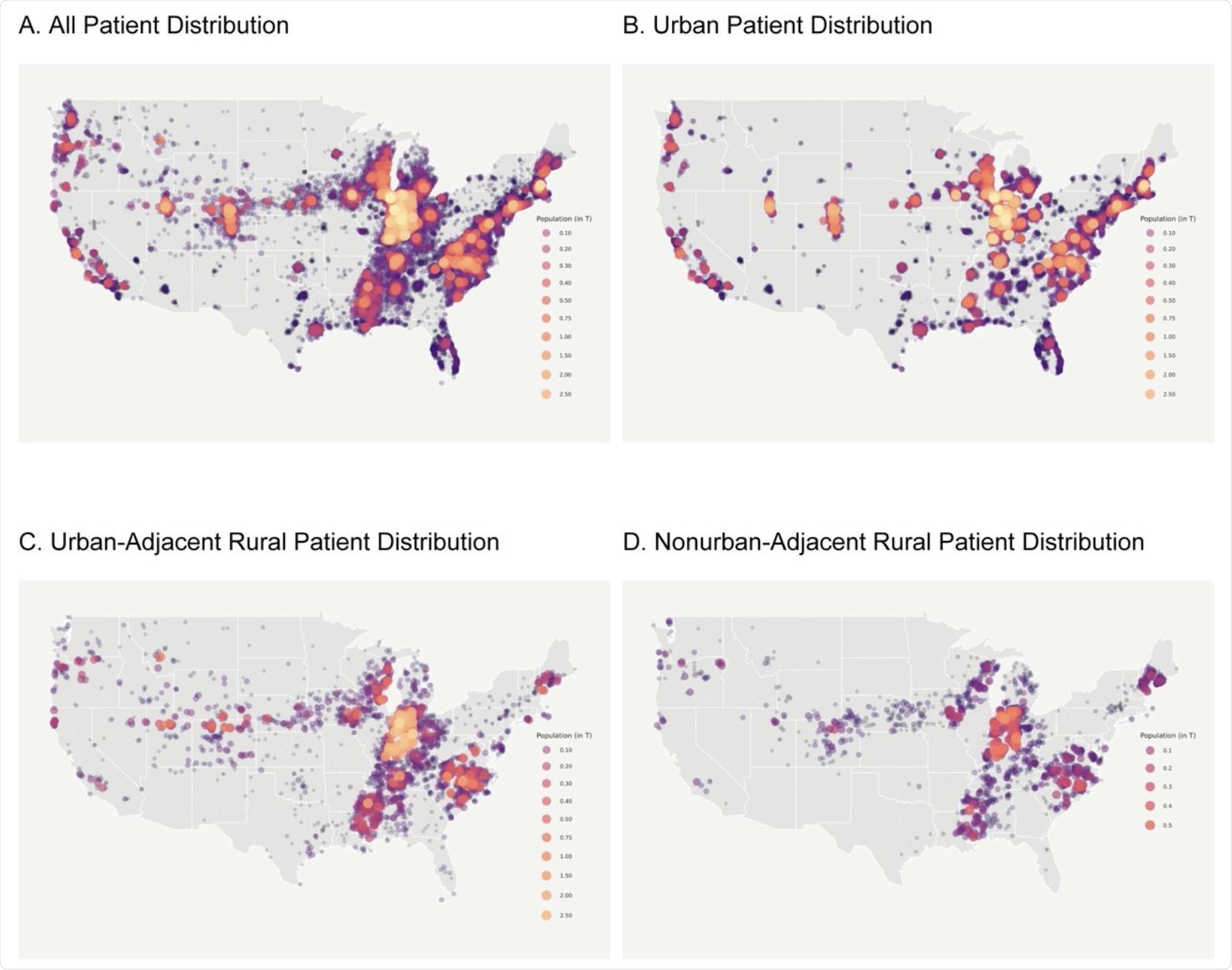 This figure shows the geospatial distribution of the N3C COVID-19 positive population. N3C contains data from 55 data contributors from across the United States, 40 of whom include sufficient location information to spatially map by ZIP Code centroid. Of those sites, we selected 27 whose data met our minimum robustness qualifications for inclusion in our study.
This figure shows the geospatial distribution of the N3C COVID-19 positive population. N3C contains data from 55 data contributors from across the United States, 40 of whom include sufficient location information to spatially map by ZIP Code centroid. Of those sites, we selected 27 whose data met our minimum robustness qualifications for inclusion in our study.
The researchers examined primary outcomes, which included hospitalization and all-cause mortality among hospitalized COVID-19 patients. Kaplan-Meier analysis and mixed-effects logistic regression were used to estimate day survival in hospitalized patients and their associations between rurality, hospitalization, and inpatient mortality.
The overall patient demographics in this study showed the rural inhabitants to be older and less racially and ethnically diverse, even in the COVID-19 negative comparison group. The rural populations had high underlying health disparities, particularly higher rates of obesity, and observable vulnerabilities including hospital visits prior to COVID-19.
After adjusting for differences in gender, race, ethnicity, body mass index (BMI), age, and Charlson Comorbidity Index (CCI), the researchers estimated an approximately 40% increased risk of hospitalization and mortality among the COVID-19 patients in the rural areas.
Significantly, higher mortality was reported 30 days after hospitalization among rural COVID-19 patients as compared to their urban counterparts. Consistent with studies on COVID-19, the study showed that hospitalized COVID-19 patients with more comorbidities, older age, and diagnosis earlier in the pandemic demonstrated significantly higher mortality.
Interestingly, comparison with patients who were not infected with the SARS-CoV-2 also resulted in similar observations, which included similar background characteristics, the likelihood of hospitalization, and greater mortality compared with urban uninfected patients. This reaffirms previous studies of the pre-COVID-19 period, where rural hospitalized patients succumbed to death at a greater rate than those from urban areas.
As compared to their urban counterparts, uninfected rural patients faced significantly higher mortality 30 days after hospitalization. The presence of underlying comorbidities also made these individuals susceptible to mortality.
The researchers also studied the secondary outcomes, which included the length of stay, supplemental oxygen, mechanical ventilation, and major adverse cardiovascular event (MACE), or extracorporeal membrane oxygenation (ECMO). The frequency for these moved higher among the rural than the urban patients.
Because the study showed that the rural versus urban effect was larger among patients hospitalized for COVID-19 than among patients hospitalized for non-COVID-19 reasons, the researchers suggested that rurality played a greater relative role in COVID-19 outcomes than it plays in the outcomes from other non-COVID-19 hospitalizations.
Conclusions
Despite adjusting for several factors, such as age and comorbidities, this study utilizes a large representative database and showed higher hospitalization and inpatient mortality rates among COVID-19 patients in the rural compared with the urban population. Thus, the current study calls for further research into the diverse factors that drive health disparities among rural populations.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Anzalone, A. J., Horswell, R., Hendricks, B., et al. (2021). Higher hospitalization and mortality rates among SARS-CoV-2 infected Persons in Rural America. medRxiv doi:10.1101/2021.10.05.21264543. https://www.medrxiv.org/content/10.1101/2021.10.05.21264543v1
- Peer reviewed and published scientific report.
Anzalone, Alfred Jerrod, Ronald Horswell, Brian M. Hendricks, San Chu, William B. Hillegass, William H. Beasley, Jeremy R. Harper, et al. 2022. “Higher Hospitalization and Mortality Rates among SARS-CoV-2-Infected Persons in Rural America.” The Journal of Rural Health 39 (1): 39–54. https://doi.org/10.1111/jrh.12689. https://onlinelibrary.wiley.com/doi/10.1111/jrh.12689.