By training, I’m a mathematical physicist and before the pandemic my research focused on the applications of topology to quantum field theory. During our first lockdown, I began talking with some colleagues at the Perimeter Institute for Theoretical Physics about how we could apply models from physics, particularly percolation theory, to understand COVID-19.
We ended up forming an interdisciplinary team of physicists alongside experts on modeling infectious diseases and vaccination. There is some classic research in percolation theory that shows that the rate of spread of an infectious disease increases when the population has more variation in their number of contacts. Our initial motivation was to better understand how these heterogeneities in human contact patterns impact public health interventions.
Image Credit: Lightspring/Shutterstock.com
The COVID-19 pandemic has taught us that by collaborating together, scientific advancements can be made quickly. How can this level of collaboration be implemented in COVID-19 vaccination programs?
This research was certainly the result of collaboration. When we were first thinking about this project our co-author Lee Smolin was wise to suggest that if we wanted to have any impact we needed to work alongside infectious disease experts.
So we teamed up with Chris Bauch, Madhur Anand, and Ed Thommes. We also added Lee’s then-PhD-student Yigit Yargic who is the other lead author of the paper and with whom I worked very closely.
Vaccines are, in some sense, inherently collaborative: They provide protection not just for the person receiving it but, oftentimes, also for those who come in contact with them. More concretely, there is certainly a need for cooperation and resource sharing to achieve equitable access to COVID-19 vaccines in all countries.
On a local scale, vaccine campaigns can be hampered by a strong degree of preferential attachment between un-immunized people, allowing the disease to spread more freely among the un-immunized. Such preferential attachment could be a symptom of division within the community around vaccination.
How do COVID-19 contract-tracing apps work?
Different countries have implemented different approaches to digital contact tracing. One popular approach uses Bluetooth to create a decentralized, encrypted contact log. The Google/Apple Exposure Notification API and BlueTrace are the two main implementations. The former is used in Canada, Europe, and some US states, while the latter in Singapore, New Zealand, and Australia.
The ‘decentralized contact log’ I referred to above is, at least in my opinion, the most exciting part of these contract tracing apps. The basic idea is that whenever two people using the app are close to each other for some time they exchange cryptographic tokens to record their contact. On each user's device there is a log listing all the contact they've had, except the entries are encrypted so that it is impossible to tell who that contact was.
When a person who has tested positive for COVID-19 chooses to upload it to the app they send out a key that allows all the other app users to decrypt the tokens they had exchanged. This is how another user’s phone can alert them to the potential exposure.
It is important to note that in the Google/Apple framework there is no way for public authorities, or anyone else, to access the encrypted contact log. These contact tracing systems operate without the central collection of private information.

Image Credit: Redkey USB/Shutterstock.com
Can you describe how you carried out your latest research into COVID-19 vaccines and contact-tracing apps?
The main technical challenge in this project was that our model needed to depend not just on how many contacts people had, but also on how long these contacts lasted. This is because of an important subtlety about how contact tracing apps record entries into the contact log.
If you spend a long time with the same person the apps could potentially exchange tokens multiple times, with new entries being added roughly every 10-15 minutes. Since the tokens are encrypted it is impossible to know whether or not two entries corresponded to contact with two distinct people or an extended or repeated contact with the same person.
The existing literature on the applications of percolation theory to infectious diseases had made the simplifying assumption that contact duration doesn’t affect the transmission probability. That is not necessarily a terrible assumption, but given how contact tracing apps work we needed time to be in the picture as well.
So, one of the things we had to do was to incorporate duration into these models and rederive the key formulas. On top of that, we had to determine how a vaccination program that prioritized individuals based on their number and duration of contacts impacted the rate of spread.
What did you discover?
A vaccine strategy that prioritizes individuals with more exposure to others has the potential to limit disease spread more efficiently. This is because people who have more contacts are both more likely to catch the disease and more likely to spread it to others. This idea has been well explored in the literature and even implemented in practice.
However, its use in the real world is limited by the ability of public health authorities to actually identify who the individuals with more contacts are. In practice, they typically make use of more coarse demographic factors. For example, in my region during a lockdown COVID-19 vaccines were prioritized for those essential workers who could not work from home because of their increased transmission risk.
We proposed a way to leverage existing contact tracing apps to more efficiently allocate vaccines. The decentralized contact log created by contact tracing apps provides a way for public health strategies, particularly vaccinations, to be aimed at high exposure individuals without the need for public authorities to centrally collect any information about the population’s contacts. In our proposal, the app makes a decision based on the number of entries in the contact log as to whether or not the app user is prioritized.
In the paper, we modeled a scenario in which demand for vaccines is much higher than supply and the aim is to achieve the greatest reduction in disease transmission from a limited supply. We considered an idealized scenario where someone receives a vaccine if and only if they are chosen by the app.
Our modeling showed that our ‘hot-spotting’ strategy using contact tracing apps reduces spread very efficiently, resulting in the ability to suppress the disease with fewer vaccines. Indeed, for our model contact network herd immunity was achieved with around half as many doses.
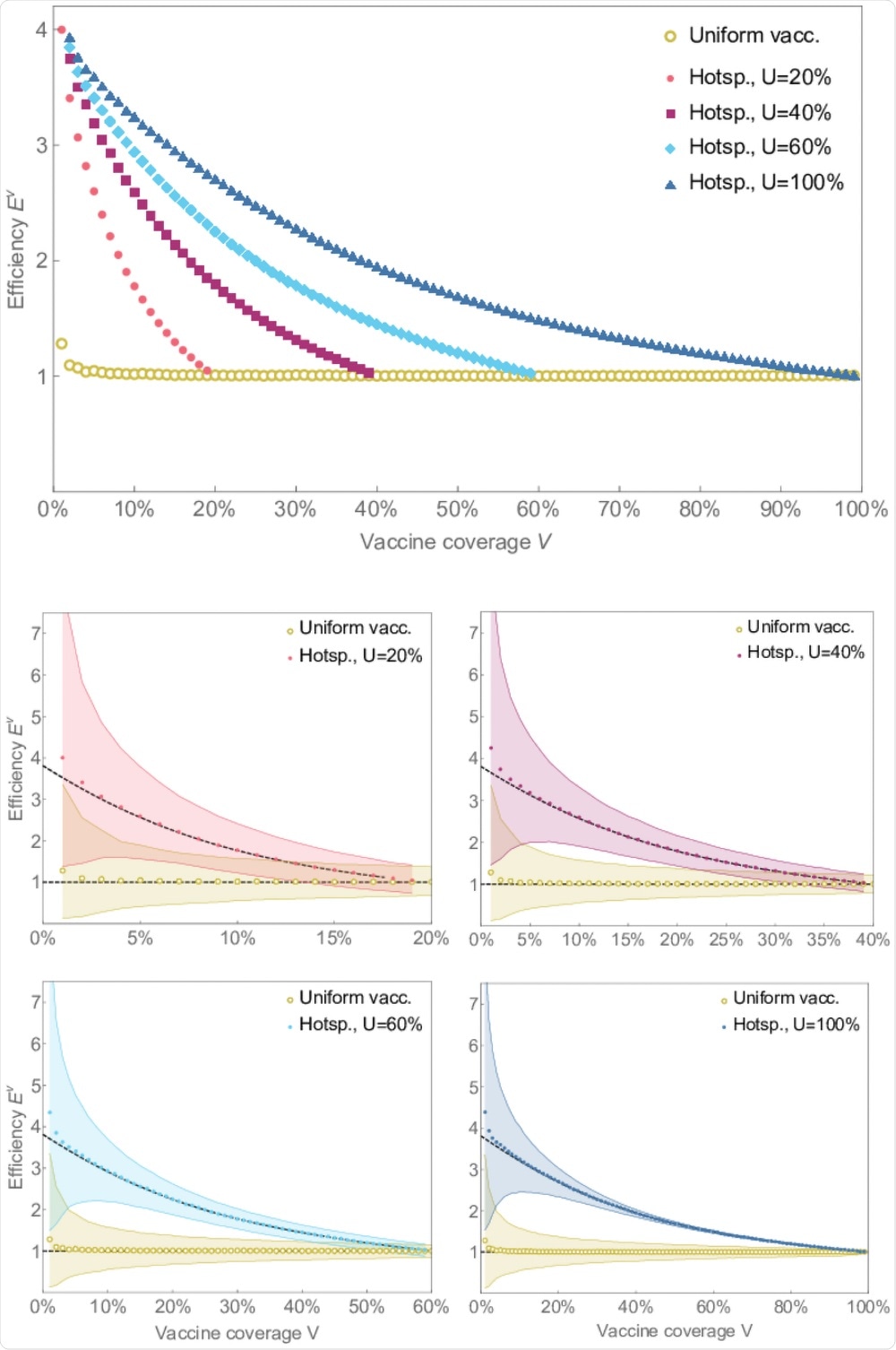
Image Credit: 2021 Penney et al
How would this approach work for developing countries where few people are using contact-tracing apps?
The fewer people who use the app the fewer people who could even potentially be chosen to be prioritized by the app. So, the total reduction in disease spread that could be achieved is limited by how many people are using the app. However, an interesting outcome of our work was that the efficiency of the strategy is still high even when the number of users is low.
Any vaccines allocated to high exposure individuals have a relatively bigger impact, and so the strategies are still able to achieve greater reductions from the vaccines that they assigned using the hot-spotting strategy.
More research would need to be done before any country can decide whether using this technology is the right solution for them. The choice of who to prioritize for vaccinations has social and health impacts beyond the rate of transmission.
Were there any limitations to your study? If so, what were they?
It would be best to think of this study as some preliminary modeling of a proposal. As mentioned above, more detailed studies would need to be done to better understand the full impacts. Having said that, there is an important limitation worth pointing out. We analyzed the app-based vaccination strategies in isolation.
In more realistic scenarios the app-based distribution would likely be occurring alongside other, more traditional systems. Indeed, to more fully understand the impact of the strategy one needs to consider it as only one part of a holistic approach to vaccination.
What is next for your research?
We’ve been building a model for a scenario more like seasonal influenza vaccination. The main driver of vaccine coverage is no longer the supply of vaccines but rather an individual choice to receive the shot. The contact tracing apps no longer serve to prioritize access to the vaccine.
Instead, when a user is selected by the app they would receive a notification promoting that they get vaccinated based on their high contact patterns. Our early results are suggesting that the hot-spotting strategy could be a valuable tool to reduce the burden of seasonal influenza, especially given its low deployment cost.
Where can readers find more information?
About Dr. Mark Penney
Mark Penney is a post-doctoral researcher at the University of Waterloo. He received his DPhil in Mathematics from the University of Oxford in 2017 for research at the interface of topology and physics. Before coming to the University of Waterloo Mark spent two years at the Max Planck Institute for Mathematics in Bonn, Germany.