The survival of coronaviruses in the community is dictated by weather conditions. It is observed that coronavirus infections are more common in winter.
 Study: Coronavirus seasonality, respiratory infections and weather. Image Credit: Dragana Gordic / Shutterstock.com
Study: Coronavirus seasonality, respiratory infections and weather. Image Credit: Dragana Gordic / Shutterstock.com
Coronaviruses
Coronaviruses (CoVs) cause respiratory and gastrointestinal infections in a variety of animals including birds, reptiles, amphibians, and mammals. Seven known coronaviruses infect humans and belong to Alphacoronaviruses and Betacoronaviruses, all of which are derived from animal sources.
SARS in 2002/2003 and SARS-CoV-2 in 2019/2020 infections started in cold dry winter seasons. Interestingly, the days that both of these infections started coincided with major national public holidays.
In the current coronavirus disease 2019 (COVID-19) pandemic, the main strategies to limit SARS-CoV-2 infection and spread included closing air travel and travel across borders, case and contact tracing, isolation or quarantine measures, implementation of social distancing, increased use of facial masks and other protective equipment, practicing diligent disinfection procedures, and implementation of strict lockdown measures.
Seasonal respiratory infections
Respiratory infections, including CoVs, are more frequent from November to March in the northern hemisphere and April to August in the southern hemisphere. A seasonal element is associated with the spread of respiratory infections. A better understanding of the seasonal changes and infections may help in designing predictive models for COVID-19.
Several mechanisms have been proposed to explain the increased rate of respiratory infections during winter. These include the effects of weather on virus survival, behavioral changes of people in winter months, and changes in people’s disease susceptibility.
Sunlight and ultraviolet (UV) exposure, for example, affects the survival of viruses on surfaces. The relative humidity is higher in winter and may thus encourage viral transmission.
Winter also results in behavioral changes, like more time spent indoors and in close proximity with other people, which may influence infection rates. Apart from these factors, low vitamin D levels due to low sunlight exposure and changes in nasal mucosal physiology due to extremes in exterior and interior temperatures may increase susceptibility to respiratory infections.
Data extraction and analysis
The authors of the current study extracted respiratory virus disease data from the Second-Generation Surveillance System (SGSS) database, which is used for routine surveillance in England and Wales. Individual cases of infectious diseases that occurred in England and Wales between 1989 and 2019 were diagnosed at a local laboratory or national reference laboratory level. The data represented laboratory diagnoses across the 31 years and included reverse-transcription polymerase chain reaction (RT-PCR) diagnoses of CoVs from 2012 to 2019.
Seasonal CoVs from this eight-year study period were compared to daily average weather parameters before the patients’ specimen date with a range of lag periods. This allowed examination of the relationship between the season and coronavirus cases.
The daily averages of weather parameters were obtained from the Met Office within a box that covers England and Wales. The weather parameters included daily averages for air temperature, dewpoint temperature, relative humidity, hourly precipitation, hourly global radiation, and sunshine.
Seasonal distribution of coronavirus infection
The authors assessed 985,524 viral infections in England and Wales in the 31-year study period. CoV infections had a seasonal distribution similar to that of influenza A and bocavirus. The seasonal distribution had a winter peak between the second and eighth week.
Of the total infections, 90% occurred when either of the following parameters existed:
- The daily mean ambient temperatures were below 10°C.
- The daily average global radiation exceeded 500 kJ/m2/h.
- The sunshine was less than 5h a day.
- The relative humidity was above 80%.
CoV infections were more common when either of the following parameters existed:
- The daily average global radiation was under 300 kJ/m2/h.
- The average relative humidity was over 84%.
- The average air temperature was below 10°C
- The sunshine was less than 4h a day.
Seasonal CoV infections in children under three years of age were more frequent at the beginning of an annual epidemic than at the end.
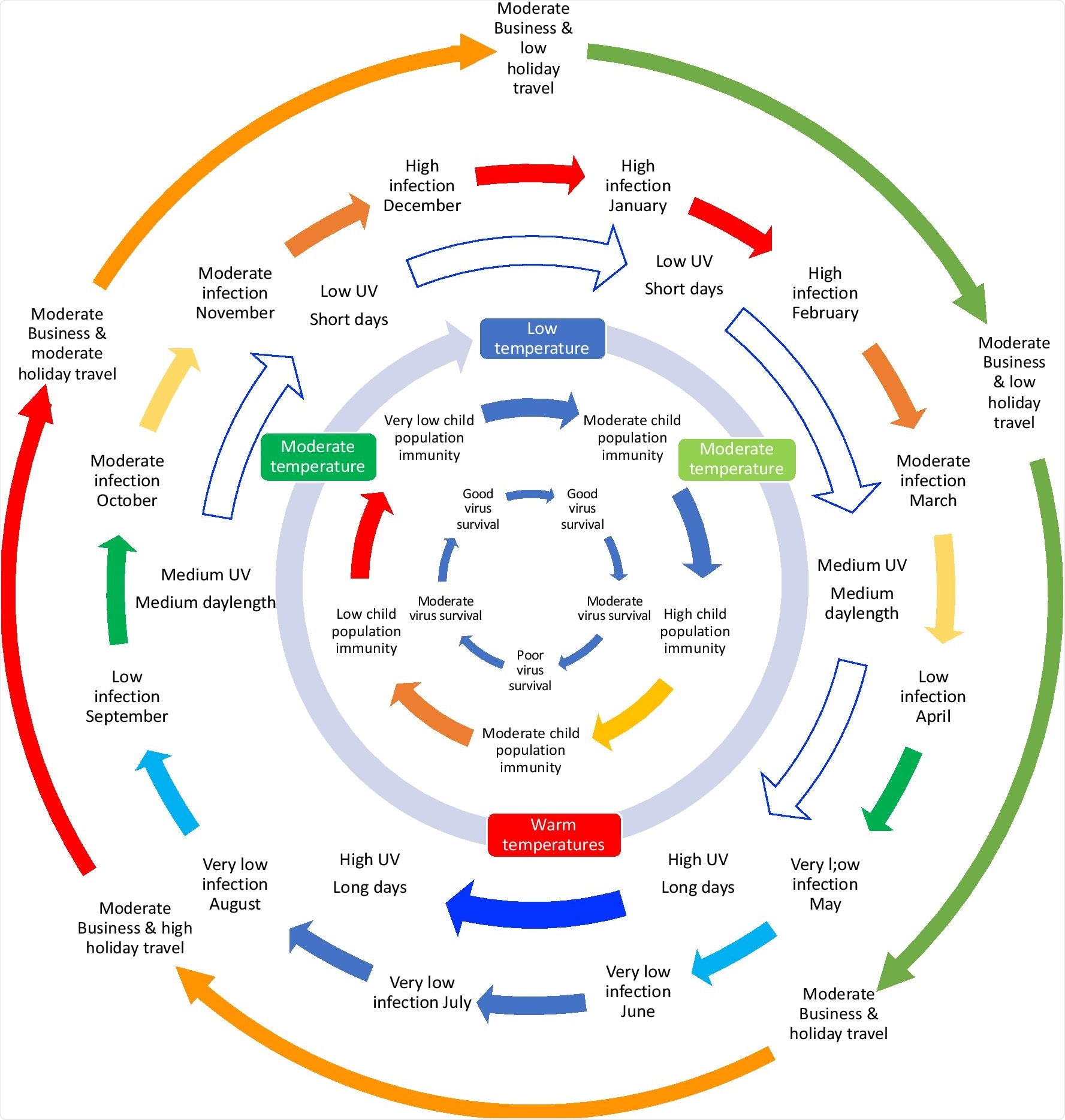 Some of the drivers influencing the seasonality of UK respiratory infections. Seasonal coronavirus infections are thought to be influenced by the size of the susceptible child population, which drives an annual epidemic in children that, in turn, infects susceptible adults. The timing of the epidemic is influenced by changing transmission dynamics through the year. Low temperature, low humidity, short daylength and low UV all probably contribute to better survival of the virus in winter months than summer, pushing the immunity driven epidemic to occur in the winter months. Travel abroad introduces new viruses that differ from the currently circulating strains. Travel variation will differ by country and holidays/festivals (including school/university holidays) (Additional file 1: S5). Many social and public interactions that contribute to infection are relatively constant through the year. In addition to these drivers there will be the gradual increase in susceptibility as a result of declining antibody levels and genetic drift within the viruses.
Some of the drivers influencing the seasonality of UK respiratory infections. Seasonal coronavirus infections are thought to be influenced by the size of the susceptible child population, which drives an annual epidemic in children that, in turn, infects susceptible adults. The timing of the epidemic is influenced by changing transmission dynamics through the year. Low temperature, low humidity, short daylength and low UV all probably contribute to better survival of the virus in winter months than summer, pushing the immunity driven epidemic to occur in the winter months. Travel abroad introduces new viruses that differ from the currently circulating strains. Travel variation will differ by country and holidays/festivals (including school/university holidays) (Additional file 1: S5). Many social and public interactions that contribute to infection are relatively constant through the year. In addition to these drivers there will be the gradual increase in susceptibility as a result of declining antibody levels and genetic drift within the viruses.
Limitations of the study
The weather data represents national weather and therefore, may not represent the local weather of the patient. An additional limitation of the current study is that in England, people mostly spend their time indoors; however, data on indoor conditions was not available for the study.
Additionally, the respiratory infections recorded may be due to pneumonia or infections in children or vulnerable patients. Furthermore, milder infections and common cold data may not be recorded and were therefore not included in this study.
It is also important to note that SARS-CoV-2 may or may not follow the pattern of other coronaviruses. Finally, the effects of weather may be direct or indirect. This study does not address this or the seasonality of weather parameters.
Conclusions
Studying the seasonal distribution of disease can help prepare healthcare systems and populations to avoid the risk of serious complications and develop timely interventions.
Survival of the virus in winter months is better due to low temperature, low relative humidity indoors, short day length, and low UV. This leads to a viral epidemic in the winter months.
A seasonal increase in SARS-CoV-2 infections may occur in the United Kingdom and countries with a similar climate. Therefore, it would be prudent to implement increased measures to reduce transmission of COVID-19 in the winter months.
Journal reference:
- Nichols, G.L., Gillingham, E.L., Macintyre, H.L., et al. (2021) Coronavirus seasonality, respiratory infections and weather. BMC Infectious Diseases 21(1):1101. doi:10.1186/s12879-021-06785-2.