The World Health Organization (WHO) declared the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak a pandemic in March 2020. To characterize the cumulative incidence of SARS-CoV-2 infection, seroprevalence studies can help by determining the prevalence of presumptive immunity.
 Study: Very high relative seroprevalence of anti-SARS-CoV-2 antibodies among communities in Bangui, Central African Republic. Image Credit: Leonid Altman / Shutterstock.com
Study: Very high relative seroprevalence of anti-SARS-CoV-2 antibodies among communities in Bangui, Central African Republic. Image Credit: Leonid Altman / Shutterstock.com

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
The detection of antibodies against the SARS-CoV-2 nucleocapsid (N) protein offers information on the history of natural infection, whereas the detection of the SARS-CoV-2 spik (S) protein can either indicate a history of spike-based vaccination or natural infection. A large-scale population-based seroprevalence study can help in determining the history of SARS-CoV-2 infection in the population, including those who were asymptomatic throughout the duration of the infection.
In 2020, many countries initiated large-scale population-based and targeted group seroprevalence studies on anti-SARS-CoV-2 antibodies. In Africa, many seroprevalence analyses have been performed to determine the anti-SARS-CoV-2 antibody levels in the population.
Seroprevalence study to evaluate cumulative immunity against SARS-CoV-2 in the population of Bangui
The authors of a recent study published on the medRxiv* preprint server performed a cross-sectional study in the city of Bangui, the capital of the Central African Republic (CAR) from July 12, 2021, to August 20, 2021. The objective of their study was to evaluate the level of cumulative SARS-CoV-2 immunity in people who were not vaccinated against the coronavirus disease 2019 (COVID-19).
A random cluster sampling method was used, in which 11 households from 25 districts were selected randomly and three members from each house were enrolled in the study. A total of 799 participants were enrolled.
The data on demographic characteristics including age, gender, residence, as well as the presence of comorbidities were collected, along with venous blood samples to estimate the level of total anti-SARS-CoV-2 antibodies. A double antigen sandwich assay kit called WANTAI SARS-CoV-2 Ab enzyme-linked immunosorbent assay (ELISA) kit was used for determining the level of SARS-CoV-2 antibodies in the serum of the participants.
Higher degree of SARS-CoV-2 exposure in Bangui
The average age of the population was found to be 27 years and was within the range of 1 year to 75 years. Male participants accounted for 45.8% of the total participants. Out of the 799 participants in the current study, 60 participants had comorbidities like diabetes or cardiovascular disease.
About 74% (592/799) of the participants tested positive for SARS-CoV-2, which was the highest prevalence to date in Africa. The seroprevalence was 66.1% (203/307) for participants aged 20 years or under, 81.8% (293/358) for 21 to 40-year-olds, 79.3% (92/116) for 41 to 60-year-olds, and 83.3% (15/18) for participants older than 61 years. Participants aged over the age of 20 showed a high risk of having positive serostatus as compared to younger participants.
No difference in the proportion of serological tests was observed between males and females. Of the 60 participants with comorbidities, 78.3% had a positive serological test. This was comparable to 72.6% of the participants without comorbidities who had a positive serological test. However, this difference was not found to be statistically significant.
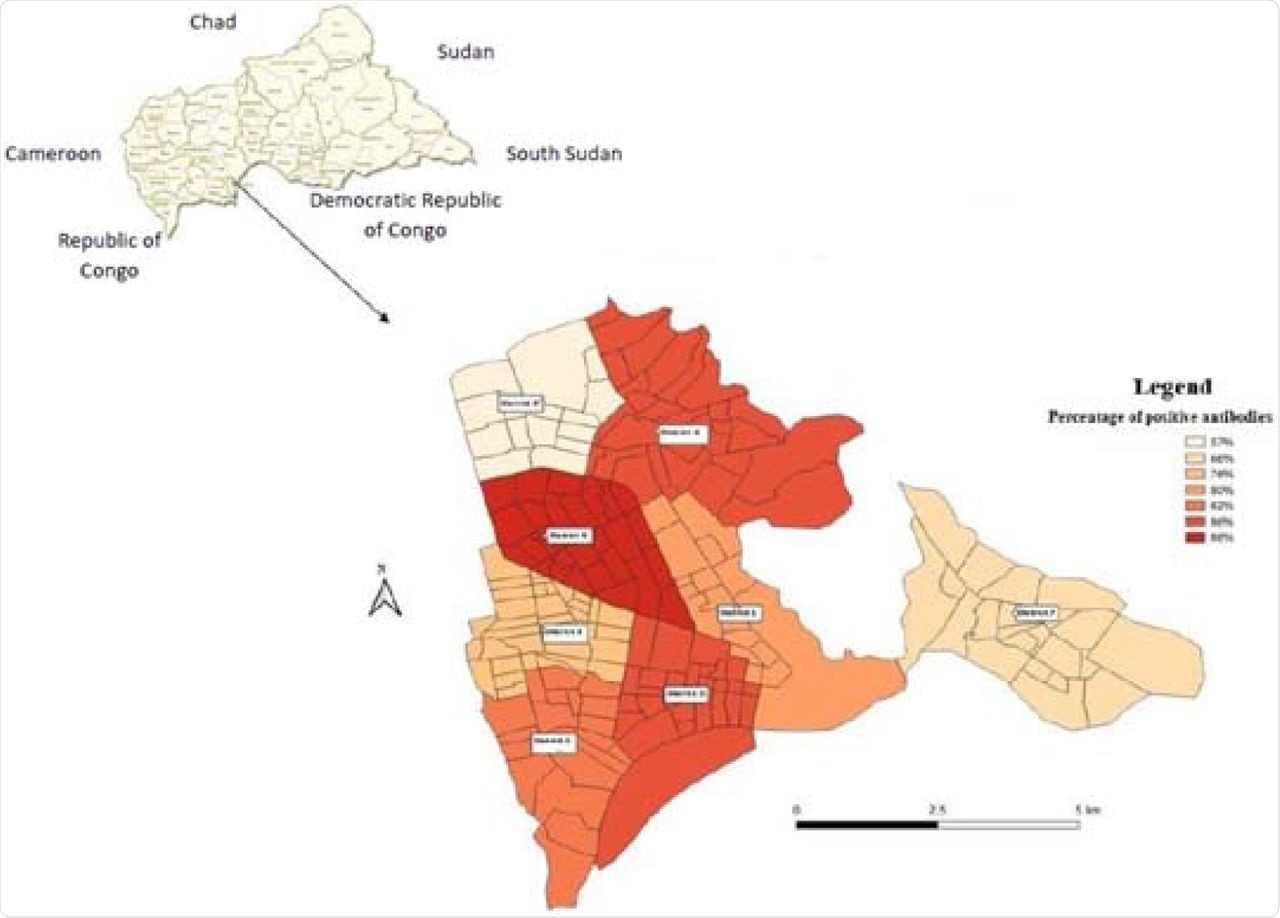 COVID-19 seroprevalence mapping in Bangui, Central African Republic, July-August 2021.
COVID-19 seroprevalence mapping in Bangui, Central African Republic, July-August 2021.
The authors observed an association between education and serological tests of the participants. The higher the education level of the participant, the more positive their serological status.
Participants with higher education levels were four times more likely to have a positive SARS-CoV-2 serological status as compared to those with lesser education levels. The authors assumed that a lack in the application of preventive measures like social distancing, sanitizing, and wearing masks are the main factors for such high seroprevalence in the population of Bangui.
Conclusions
The overall findings revealed that the population of Bangui exhibits a very high degree of exposure to SARS-CoV-2. The education level of individuals also appears to have an impact on the application of COVID-19 preventive measures.
The prevalence of a positive serological status for SARS-CoV-2 increases with age. Taken together, these findings revealed a high cumulative level of immunity and a great degree of exposure to SARS-CoV-2 in the Bangui population.
The public health implications of cumulative immunity have yet to be determined, specifically in terms of the need to vaccinate target groups or the whole population. The authors suggested more comprehensive seroprevalence studies for SARS-CoV-2 in Bangui and other regions in CAR to evaluate progressive changes in the cumulative immunity of the population and the impact of different emerging variants of SARS-CoV-2 on the gained immunity.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.