Coronavirus disease 2019 (COVID-19) related studies show that about 10% of COVID-19 patients, especially the hospitalized patients, experienced symptoms beyond three to four weeks and, in more than 75% of hospitalized COVID-19 patients, at least one symptom persists for more than six months. Some studies reported the residual effects of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, which included shortness of breath, joint pain, chest pain, cognitive disturbances, fatigue, and a drop in quality of life.
The evidence available so far suggests that many COVID-19 patients experienced prolonged/persistent symptoms, also known as Long COVID. In South Africa, a continuous rise in infection among frontline health workers has been observed since the first case of COVID-19 was reported on March 5, 2020. The advent of COVID-19 has also been noted in health care workers at Right to Care (RTC) South Africa, a Non-profit Organization operating across seven provinces providing health services.

Study: Persistent Symptoms Among Frontline Health Workers Post-acute COVID-19 Infection. Image Credit: Cryptographer/Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The study
In a pre-print study published on the medRxiv* server, the authors aimed to identify the persistent/Long COVID symptoms experienced by frontline workers at RTC South Africa, who had the acute phase of illness. The study included an anonymous cross-sectional survey conducted on an online platform from 15th February to 15th April 2021 in South Africa. The staff of RTC who worked across seven provinces (Gauteng, Free State, Eastern Cape, Northern, North-West, and Mpumalanga) in South Africa and had tested positive for COVID-19 was eligible to participate in the survey.
The survey included a questionnaire consisting of 67 items covering the following seven criteria: (1) demographics (age, sex, and ethnicity), (2) general health status (smoking, alcohol, and recreational drug use), (3) comorbidities, (4) health status at the time of COVID-19 diagnosis, (5) health status post-COVID-19, (6) current health status post-COVID-19, and (7) physical activity.
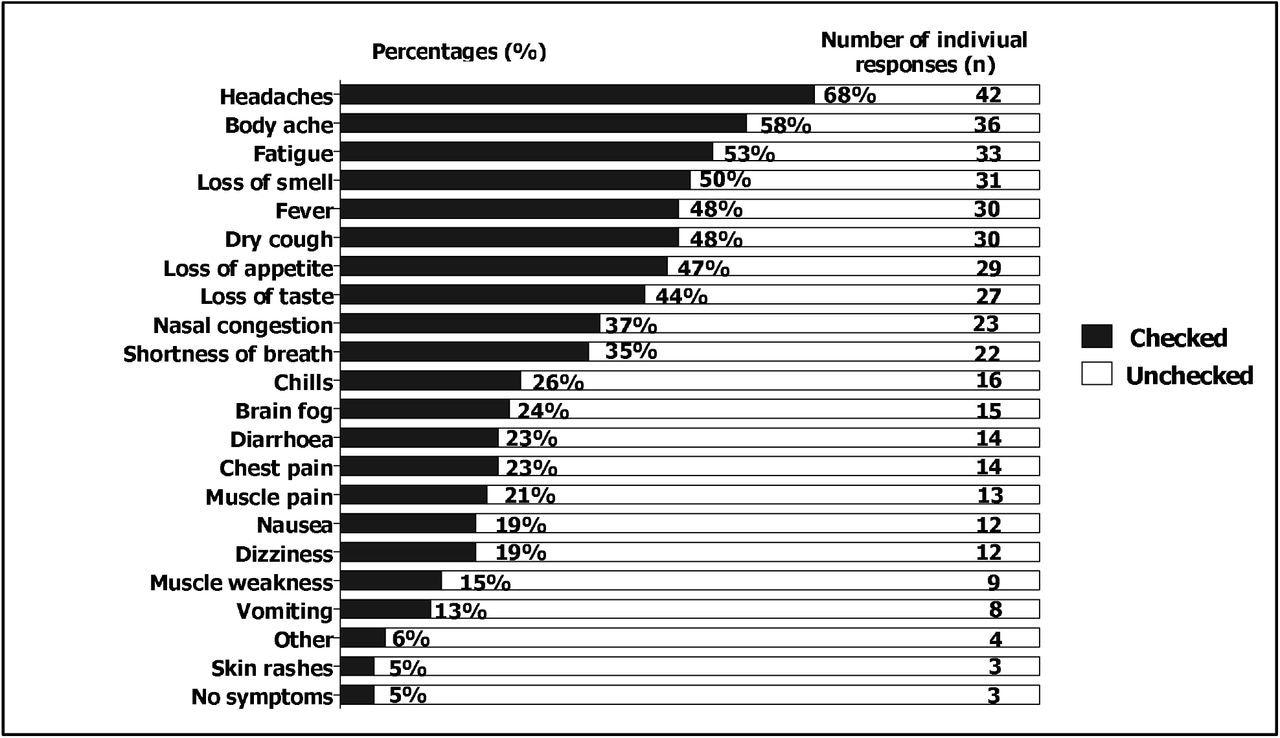 Acute COVID-19 symptoms at time of diagnosis
Acute COVID-19 symptoms at time of diagnosis
The participants reported the aggravation of post-COVID-19 symptoms using a 10- point end-labeled adopted response scale. Also, the severity of current post-COVID-19 symptoms was reported in a 10-point end-labeled slider scale. In addition, an eight-point Likert scale was used for reporting the number of days spent on an exercise prior to COVID-19 diagnosis whereas a nine-point Likert scale was adopted for the response scale on the time (in minutes) spent on an exercise according to WHO recommendation. Detailed information pertaining to the characteristics of respondents, underlying medical conditions, post-COVID-19 as well as persistent (Long) post-COVID-19 symptoms and physical activity levels were evaluated.
Key findings
In this study, 916 employees were tested for COVID-19; however, only 62 consented and completed the survey. Among 248 staff who tested COVID-19 positive, approximately 38% (n=95) and 17% (n=42) were community/field health workers and medical/clinical personnel, respectively. The results of the study showed that more than a third of the respondents had persistent symptoms beyond four weeks. It was also found that all frontline cadres, especially community health workers and medical/clinical personnel had been positively affected by COVID-19 since its appearance in South Africa.
The survey showed hypertension as a common comorbid condition among respondents and 47% reported persistence in at least one symptom, particularly fatigue, anxiety, brain fog, muscle pain, and difficulty in sleeping. Also, the findings of the study revealed fatigue as the most reported persistent and bothersome symptom post-acute SARS-CoV-2 infection. In addition, no association was established between hypertension and fatigue or the other reported persistent symptoms.
It was also found from the data that the reduction in physical activity could be attributed to lockdown regulations put in place in the first and second waves of the infection. A major limitation of the study is the small sample size of positive cases for the SARS-CoV-2 diagnostic test result which reduces the statistical power to identify Long COVID risk factors.
Conclusion
In conclusion, the findings show that persistent/Long COVID-19 among frontline workers could directly impact health service delivery. The study highlighted the significance of reducing the spread of COVID-19 through validated public health measures and vaccinations and continued research into Long COVID to find rehabilitation/treatment options.
Consistent with existing findings, fatigue was the most reported persistent and bothersome symptom post-acute SARS-CoV-2 infection.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Constance Wose Kinge, et al. 2021. Persistent Symptoms Among Frontline Health Workers Post-acute COVID-19 Infection. medRxiv. doi: https://doi.org/10.1101/2021.12.03.21267225 https://www.medrxiv.org/content/10.1101/2021.12.03.21267225v1
- Peer reviewed and published scientific report.
Wose Kinge, Constance, Susan Hanekom, Alison Lupton-Smith, Francis Akpan, Eula Mothibi, Thapelo Maotoe, Floyd Lebatie, Pappie Majuba, Ian Sanne, and Charles Chasela. 2022. “Persistent Symptoms among Frontline Health Workers Post-Acute COVID-19 Infection.” International Journal of Environmental Research and Public Health 19 (10): 5933. https://doi.org/10.3390/ijerph19105933. https://www.mdpi.com/1660-4601/19/10/5933.