I wanted to investigate, in a large patient series, the full extent of CNS complications and an accurate incidence of these non-pulmonary complications. I used my large network of scientific colleagues in the USA and in Europe to investigate this important topic.
Since the start of the COVID-19 pandemic, much research has looked into the pulmonary problems related to COVID-19 but there has been little research into other organs that may be affected. Why is this and why is it important to investigate COVID-19’s impact on all organs of the body?
The pulmonary complications are well understood however COVID-19 can affect the entire body including the brain. Some of these brain complications cause immediate and severe brain complications such as strokes and bleeding in the brain.
Image Credit: Vitalij Terescsuk/Shutterstock.com
Previous literature into central nervous system (CNS) complications only focused on a small number of hospitalized COVID-19 patients. However, your new study is the largest multi-international study to date that focuses on this. What is the importance of having a large patient database and how does this affect the accuracy of your conclusions?
It is important to investigate a large database so the full extent of the disease complications can be understood and an accurate incidence of these complications can be determined.
Can you describe how you carried out your latest research into COVID-19 and brain complications? What did you discover?
We investigated almost 40,000 patients that were admitted to a hospital for COVID-19.
Approximately 10 percent of these patients had either a CT or MRI imaging study of their brain due to a possible neurologic problem. In this group of patients that were imaged, approximately 10 percent were found to have significant brain complications.
Overall approximately 1.2% of hospitalized COVID-19 patients developed significant CNS complications.
What were some of the most common CNS complications that you discovered?
The most common brain complications were: strokes and brain bleeding, followed by brain inflammation, sinus venous thrombosis, acute demyelinating encephalomyelitis, posterior reversible encephalopathy syndrome, and vasculitis.
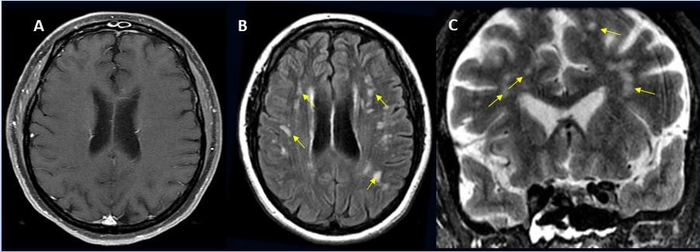
Image Credit: Radiological Society of North America and Scott H. Faro, M.D.
Your research all showed the similarities and differences between patients in the USA and Europe. Please could you describe some of these similarities and differences and why these might have been observed?
- CVA was more common in the USA (74%) versus Europe (40%). This may be in part due to a significant difference (p=0.02) in the incidence of comorbidities (cardiac, diabetes, chronic renal failure) in the American population (31.6%) compared to our European population (21.3%)
- In our study bleeding in the brain, Encephalitis, and ADEM were more common in Europe.
- The prior literature investigated a significantly lower number of hospitalized Covid-19 patients which limited the determination of accurate incidences of CNS complications
- In our cohort of ~ 40K - The overall incidence of CVA in the total population was lower c/w the literature (0.7% v 1%)
- Overall approximately 1.2% of hospitalized Covid-19 patients develop significant CNS complications. That means that a little more than one out of every 100 patients that are admitted to a hospital for COVID-19 will have a significant abnormality in their brain.
How will your research help to further improve our understanding of COVID-19’s complications on the body?
Being aware of non-pulmonary complications is very important so a holistic approach to patients care can be performed. Additionally, many of the brain complications are life-threatening and need special treatment.
Clinicians should have a low threshold to order brain imaging in COVID-19 patients if there is any question of a possible neurological disorder.
Do you believe that with continued research into COVID-19, we will discover more complications concerning other organs also?
I am sure more complications will be discovered as COVID-19 is a devastating viral disease that affects the entire body.
What are the next steps for you and your research?
To further understand the differences between the incidences of CNS complications between regions in the world with respect to specific strains of COVID-19 viruses, issues related to healthcare access and regional ordering of advanced brain imaging, and finally to investigate the complications of the spine related to COVID-19.
Where can readers find more information?
About Professor Scott H. Faro
I am currently a professor of radiology and neurology and director of Neuroradiology and Head and Neck Radiology at Thomas Jefferson University. The focus of my academic medical carrier has been to advance translational neuroimaging research that can create new imaging techniques that then can be used in the clinics and to teach these state-of-the-art imaging procedures to my radiology residents, neuroradiology fellows, and my colleagues. 
I am a founding member and past president of the American Society of Functional Neuroradiology and senior editor of several textbooks including a comprehensive book: Functional Neuroradiology: Principles and Clinical Applications, soon to be in the second edition.