A recent study by a team of European researchers demonstrated how antibodies induced by currently circulating influenza A H1N1 strains can cross-react with the important part of the SARS-CoV-2 spike glycoprotein that interacts with the human cell receptor. Their paper is currently available on the medRxiv* preprint server while it undergoes peer review.
The susceptibility to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of the coronavirus disease 2019 (COVID-19), can differ substantially among different individuals, alongside the clinical presentation of the disease.
More specifically, studies looking at the original strain showed how approximately 50% of infections are asymptomatic; furthermore, among those with symptoms in Sweden, 80% of them were mild, and 3-5% of individuals have been admitted to the intensive care unit.
Of course, since the start of the COVID-19 pandemic, there have been many different variants where these percentages could differ, but one possible explanation for such variability in disease susceptibility/severity can be found in prior protective immune responses.
This study, led by two first authors from Karolinska Institutet in Stockholm (Sweden), hypothesized that the pattern of diminished viral spread and the evident protection of approximately 80% of the population from severe COVID-19 could be linked to a pre-existing immunity that also contributes to herd immunity thresholds.
Testing the hypothesis
To test this hypothesis, the study groups applied mathematical models to appraise the effects of various factors, such as age, mobility, previous immunity, interactive patterns, as well as introduced nonpharmacological interventions.
The researchers have also tested the ability of pre-existing antibodies to inhibit binding of the spike glycoprotein to the angiotensin-converting enzyme 2 (ACE2) receptor in a SARS-CoV-2 surrogate viral neutralization test.
Levels of antibodies against a specific NGVEGF peptide have also been evaluated with an enzyme-linked immunoassay (ELISA) diagnostic method on a sample of 328 healthy individuals (primarily blood donors) from Sweden and predicted T cell responses have also been evaluated in depth.
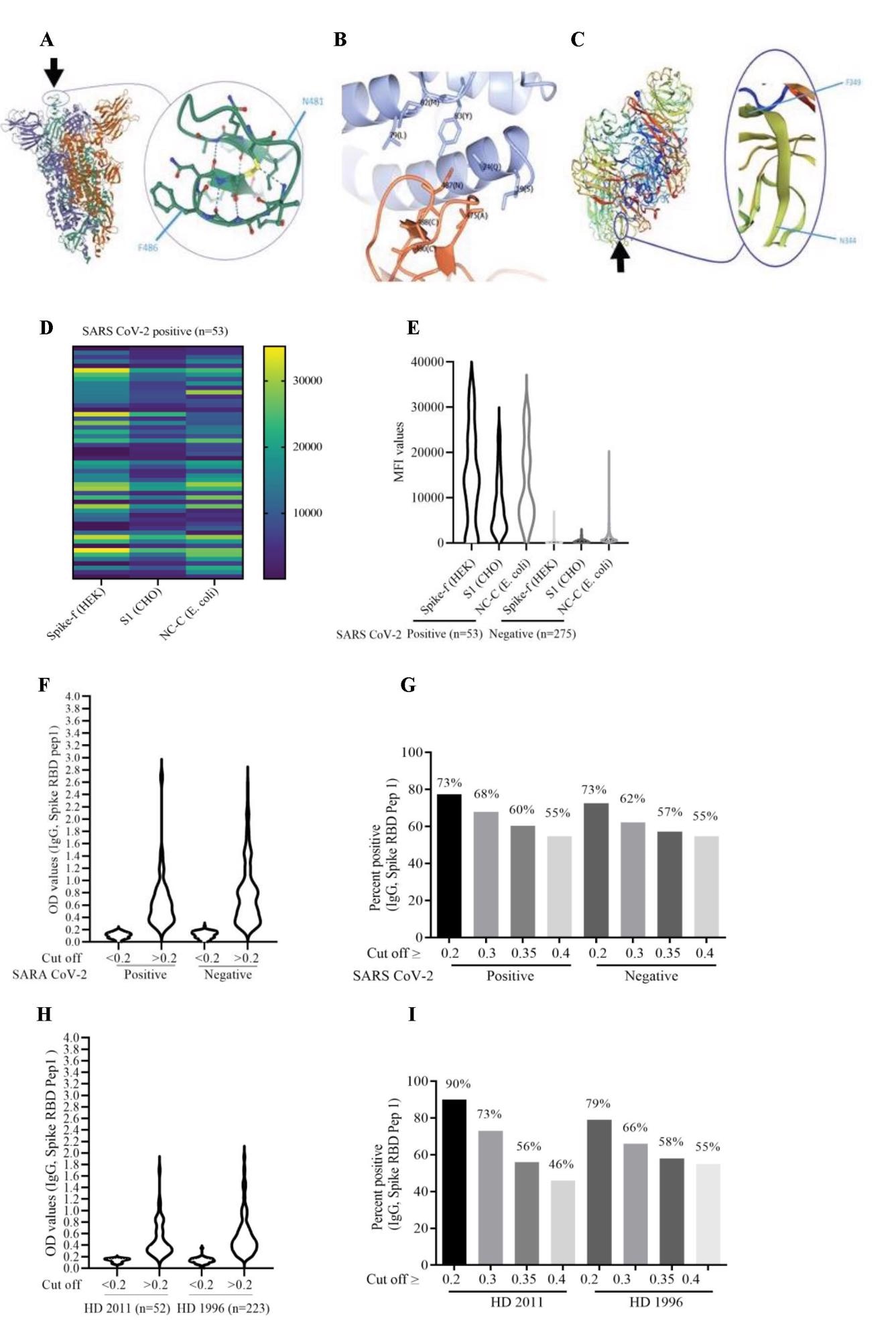
Heat map showing peptide-specific IgG antibodies and bead array assay data (MAD) in COVID-19-positive and COVID-19-negative individuals. (A and C) Heat map of MAD values for peptides 3, 7, and 11 in COVID-19 positive (A) and COVID-19-negative (C) cohorts. (B and D) The IgG antibody levels (MAD values) to the NGVKGF (peptide 7) were higher than to the NGVEGF peptide (peptide 3) in both COVID-19-positive (B) and COVID-19-negative (D) cohorts. (E–H) Peptide-specific IgG antibodies in two COVID-19-positive individuals (E and F), in a subject who was exposed to Flu and SARS CoV-2 but did not get sick (G), and in a COVID-19-negative subject (H). ****p<0.00001, ***p<0.0001, **p<0.001, *p<0.01, ns: not significant.
A robust cross-protection against SARS-CoV-2
Approximately 58–68% of blood donors in Stockholm (Sweden) had detectable antibodies to the tested cross-reactive peptide, NGVEGF, while seasonal influenza vaccination tended to enhance the binding of inhibitory antibodies to SARS-CoV-2. In addition, this peptide has also activated T-cell immunity in 20% of healthy individuals.
Furthermore, eleven additional T-cell peptides with the propensity of cross-reacting with influenza and SARS-CoV-2 have been identified, with the potential to protect against SARS-CoV-2 in up to 71% of individuals.
These findings may explain why so many people in Sweden have not been infected after evident household exposure or presented with asymptomatic or mild infections. But, naturally, newly emergent strains may rapidly change the landscape.
Implications within the epidemiological context
These models support the hypothesis that pre-existing immunity to influenza A H1N1 strains can confer protection for a wide array of people from SARS-CoV-2 infection – and that even vaccination against seasonal flu adds another layer of safety.
Regarding the latter, different epidemiological studies have demonstrated that seasonal influenza vaccination provides substantial protection against COVID-19, and especially severe forms of the disease necessitate hospitalization and/or admission to the intensive care unit.
“Such immunity is not expected to provide sterilizing immunity to SARS-CoV-2”, say study authors in this medRxiv paper. “Rather, it acts as a brake on the epidemic spread, as a higher viral dose is needed to infect someone who has a substantial level of flu-mediated pre-immunity under current nonpharmacological interventions,” they add.
These findings are important for understanding the nature of SARS-CoV-2 susceptibility, the highly individual natural course of COVID-19, protection against novel variants, vaccine response, and the overall impact of the virus on our society.