Immune aging is a phenomenon strengthened by the multifaceted remodeling of both innate and adaptive immunity. This includes lower antigen responses, decreased memory T cell response as well as a persistent chronic inflammation. Furthermore, immune aging also leads to more severe consequences of viral infection and lower protection post-vaccination.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The severe acute syndrome coronavirus 2 (SARS-CoV-2) infection that is the cause of the ongoing COVID-19 pandemic is known to have a more significant impact on older adults leading to higher mortality, increased hospitalizations, prolonged disease, and delayed viral clearance.
Currently, vaccination is the most effective precautionary measure for the severe symptomatology caused by SARS-CoV-2, especially for the elderly population. The BNT162b2 mRNA vaccine (Biotech/Pfizer) has been shown to have high safety and efficacy against serious SARS-CoV-2 infections. Double doses of this vaccine induced a robust humoral response due to the production of neutralizing antibodies. Additionally, SARS-CoV-2 S-specific CD4+ and CD8+ T cell responses have also been observed following vaccination with the BNT162b2 vaccine.
Although the BNT162b2 vaccine was found to be quite effective, lower effectiveness was observed in the case of older adults infected by
SARS-CoV-2. Several studies have also shown lower levels of neutralizing antibodies in vaccinated older adults, especially six months post the second dose. Also, more inadequate S-specific T cell responses have been observed in the case of vaccinated elderly individuals.
A new study posted to the pre-print server medRxiv* investigated the significant immune alterations concerning SARS-CoV-2 specific innate and adaptive immunity associated with a lower BNT162b2 mRNA vaccine response in older individuals.
About the study
The study involved a total of 54 participants who were vaccinated with the BNT162b2 mRNA vaccine. Participants were excluded if they were diagnosed with dementia, had active infections, or were hospitalized during the last six months before the study. In addition, participants with a positive SARS-CoV-2 specific PCR test and those with detectable anti-SARS-CoV-2 antibodies before vaccination were also excluded from the study. The participants taking part in the study were categorized into young (less than 60 years) and old (60 years or above) subjects.
Peripheral blood samples were collected from the patients from February to November 2021. The innate and adaptive immunity was studied at three-time points, before the administration of the first dose (PRE), three weeks after the first dose, just before the administration of the second dose (1D), and two months after the second dose (2D).
Peripheral blood mononuclear cells (PBMCs) were isolated from the participant’s blood and used to analyze the SARS-CoV-2 specific T cell response, monocytes stimulation, myeloid dendritic cells stimulation, and quantification of IFN-α production. Multiparametric flow cytometry was carried out for ex vivo phenotyping and functional assays followed by quantification of anti-RBD IgG SARS-CoV-2 levels. Finally, DNA was extracted from the PBMCs and sj/β TREC was measured using digital droplet PCR (ddPCR).
Study findings
The results indicated no significant differences in the production of SARS-CoV-2 specific IgG levels after administration of the vaccine were observed in young and old subjects. However, an inverse relationship between anti-RBD IgG levels and age was observed after the administration of the first dose as compared to the second dose.
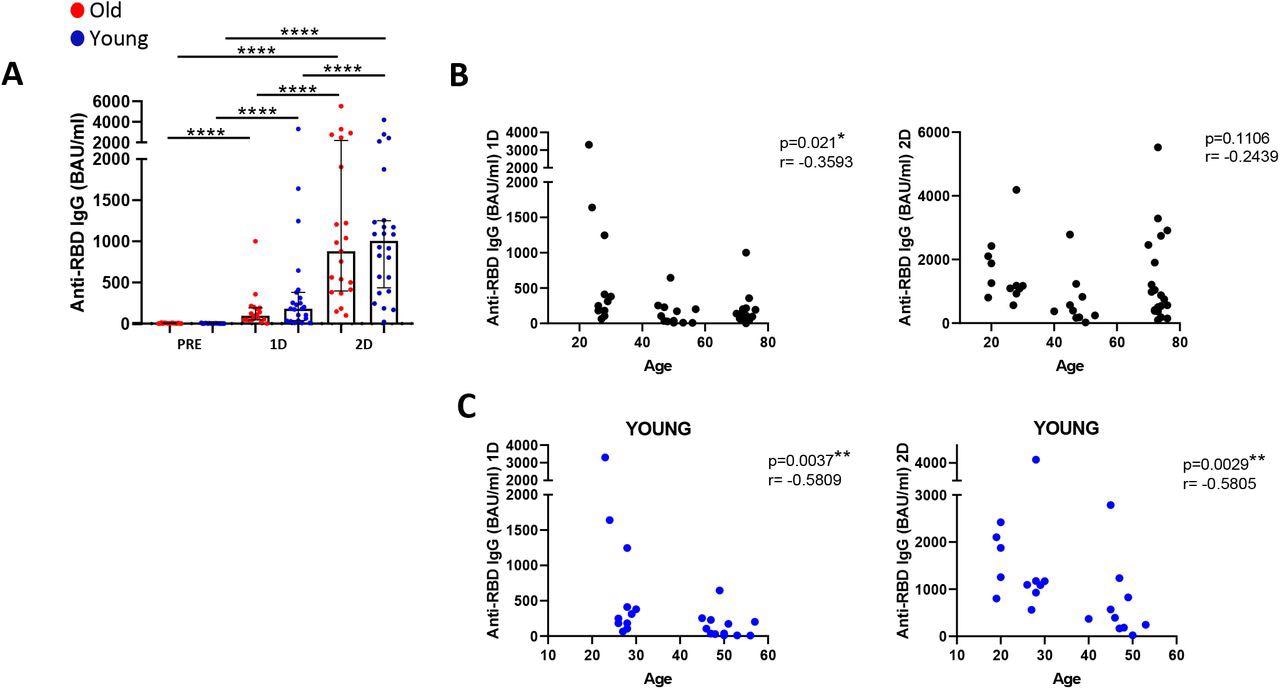
SARS-CoV-2 specific IgG levels are inversely associated with age (A) Anti-RBD IgG levels (Binding Antibody Units (BAU)/mL) in old and young participants before SARS-CoV-2 vaccination (PRE), three weeks after the first dose (1D) and two months after the second dose (2D). (B and C) Correlation of anti-RBD IgG levels with age in all the study participants (B) and only in young group (C) after the first dose (left panels) and after the second dose (right panels).
The results reported that three weeks following vaccination with the first dose, CD4+ T cells produced interferon-gamma (IFN-γ) and tumor necrosis factor-alpha (TNF-α) as well as low levels of the degranulation marker CD107a, perforin (PRF), and interleukin (IL)-2. However, lower SARS-CoV-2 S-specific IFN-γ production and the cytotoxic response were observed in older adults post-vaccination. A similar observation was reported concerning CD8+ T cell response in older adults. Moreover, a low polyfunctional memory CD4+ T cell response was observed in older people compared to younger ones.
The results also indicated lower levels of thymic function in older adults as compared to young individuals. Decreased thymic function leads to memory inflation that alters the proportion of the naïve and memory T cells. Additionally, due to lower thymic function and high memory inflation, high levels of T cell homeostatic proliferation and activation were observed in older individuals. Vaccination also increased the expression of the immune checkpoints on CD4+ and CD8+ T cells in young individuals as compared to the older ones. Also, higher CD161+ T cell levels were observed in young people as compared to the senior participants.
Furthermore, a decrease in plasmacytoid dendritic cells (pDCs) two months after administering the second dose of the vaccine was observed. Upon stimulation of pDCs, lower levels of IFNα production were observed in the case of older adults as compared to young ones after both doses of vaccine. Characterization of myeloid dendritic cells (mDCs) including CD1c+, CD16+ and CD141+ mDCs was also carried out. Higher levels of CD16+ and CD1c+ were observed in young people as compared to the older adults while no difference in the level of CD141+ was observed for both groups.
Finally, the results also reported an increase in the expression of activation markers in classical and intermediate monocytes upon vaccination in young people as compared to older participants. A decrease in classical monocytes following two vaccine doses has been observed only in older participants. Also, upon LPS stimulation, older people were found to produce higher levels of proinflammatory cytokines. Additionally, participants who did not show a cytotoxic SARS-CoV-2 specific T cell response (PRF-) were observed to produce higher levels of inflammatory cytokines by monocytes post-vaccination.
Therefore, the current study demonstrates the age-related immune deficits that exist in older adults. Furthermore, the results of the study provide a better understanding of why the vaccine responsiveness against SARS-CoV-2 is lower in older individuals, which can help in the improvement of current vaccination strategies as well as help to develop more efficient prototypes for the general population.
Limitations
The study had certain limitations. First, the sample size for the study was small. Second, a longer follow-up could be helpful in the determination of the impact of vaccination. Finally, a response against only the BNT162b2 mRNA vaccine was included in the study.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources