Studies show that newly emerging SARS-CoV-2 variants of concern (VOCs) like Alpha, Beta, Delta, and Omicron differ in vital aspects, including the viral entry mechanism and evading the human immune response. However, there is insignificant data regarding the impact of these differences on the infectivity and neutralization of the virus.
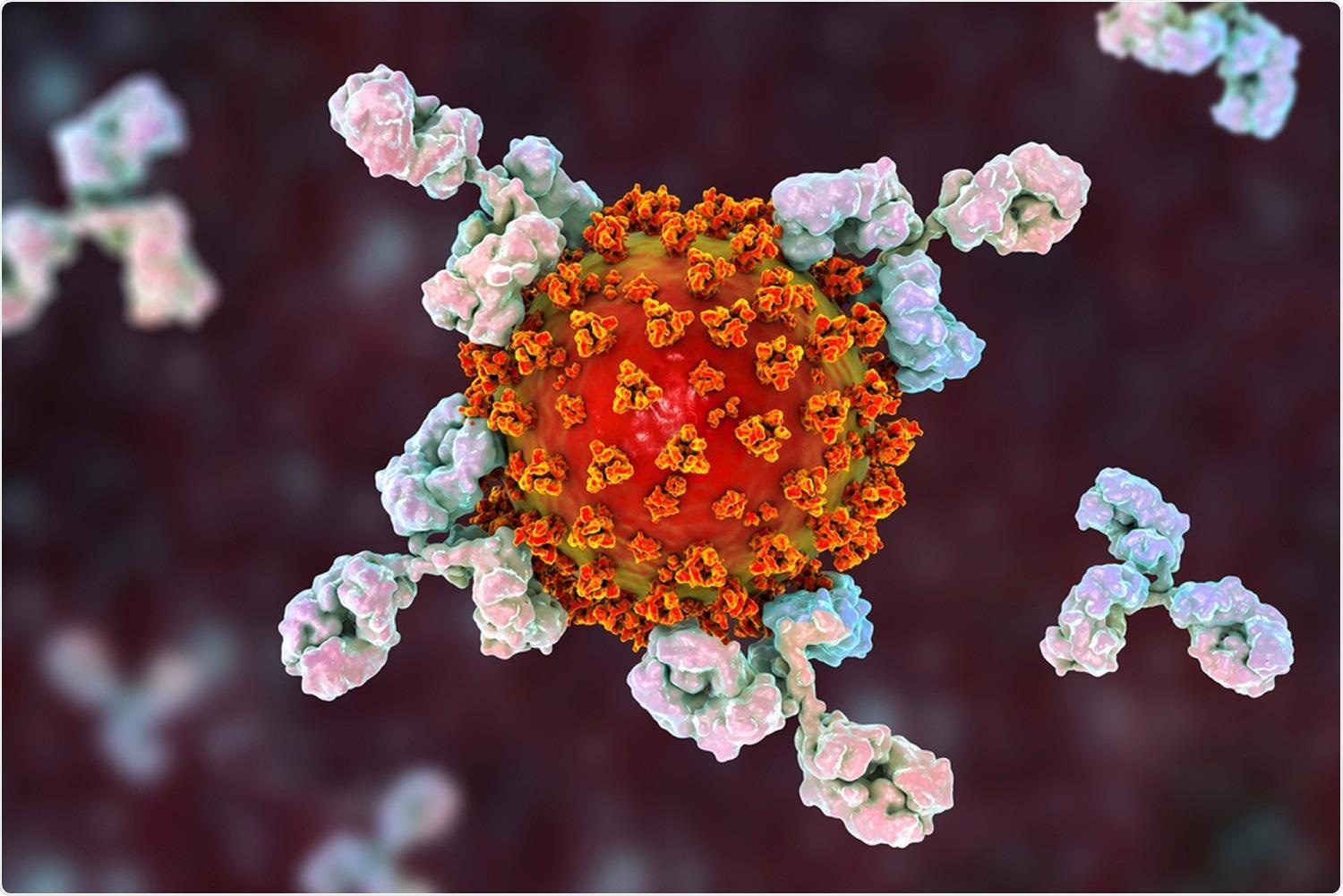 Study: Impact of New Variants on SARS-CoV-2 Infectivity and Neutralization: A Molecular Assessment of the Alterations in the Spike-Host Protein Interactions. Image Credit: Kateryna Kon / Shutterstock
Study: Impact of New Variants on SARS-CoV-2 Infectivity and Neutralization: A Molecular Assessment of the Alterations in the Spike-Host Protein Interactions. Image Credit: Kateryna Kon / Shutterstock
About the study
The present study examined the interactions of SARS-CoV-2 VOCs with essential proteins that impact entry of the infectious virus in the human host and their ability to evade neutralizing monoclonal antibodies (mAbs).
The study involved in silico mutagenesis and examination of structural models of SARS-CoV-2 spike (S) glycoprotein receptor-binding domain (RBD) of the VOCs, which were complexed with angiotensin-converting enzyme 2 (ACE2) and Abs. Structural models of five mutant RBDs - including N501Y (Alpha); K417N, E484K, and N501Y (Beta); L452R and T478K
(Delta); E484K; double mutant E484K and N501Y (UK2)- complexed with ACE2 were generated.
A series of molecular dynamics (MD) simulations were performed to examine the impact of N-linked glycans and disulfides on viral mechanisms. The trajectories of MD simulations for RBD-ACE2 protein−protein complexes were taken in an explicit solvent. Ions, molecules, and glycans were removed from the MD solution, which resulted in trajectories for ACE2. RBD, and the RBD-ACE2 complex. The molecular mechanics/generalized Born surface area (MM/GBSA) free energy of these resulting trajectories was calculated.
The binding energetics of the RBD-ACE2 complex were evaluated with three methods namely, PRODIGY; PRODIGY refined by HADDOCK, and the MM/GBSA method. The binding energies of the Abs produced by the RBD-ACE2 complex were calculated using an anisotropic network model (ANM). The RBDs of both SARS-CoV-2 wild type (WT) strain and Delta VOC were analyzed with the enzyme-linked immunosorbent assay (ELISA)
Results
The study results showed that N501Y RBD residues shared by SARS-CoV-2 Alpha, Beta, UK2, Gamma, and Omicron VOCs, increased ACE2 binding and, thus, the infectivity of the virus. The RBD-ACE2 model for the Alpha VOC had a root-mean-square-deviation (RMSD) of 0.9 Å as opposed to RMSD of 1.0 Å in the Beta RBD-ACE2 model. N501 RBD also formed stable interactions with ACE2 residues K353 and Y41, which regulated ACE-2 binding to SARS-CoV S RBD.
Van der Waals interactions were found to play an important role in the formation of ACE2-RBD complexes in the Alpha VOC and UK2 while solvent-accessible surface area (SASA) and electrostatic effects improved the stability of the complex in Alpha. The evaluation of binding free energy showed that the Alpha, UK2, and the Beta VOCs had a higher affinity towards ACE2 binding as compared to the WT strain RBD.
The K417 RBD in the Beta and Gamma VOCs was more specific to SARS-CoV-2 than SARS-CoV. The highly stable salt bridge between this RBD and ACE2 facilitates the formation of a complex between the two components. Local conformational changes caused by the N501Y mutation also stabilizes the salt bridge between the RBD-ACE2 complex. In contrast, K417N and K417T mutations, respectively, reduce the binding affinity of the RBD to ACE2 in Beta and Gamma VOCs.
The E484 RBD was found in a loop region that was subjected to conformational fluctuations and consists of a potential disulfide bridge that reduced RMSD. The ACE2 binding enthalpy of the Beta and the Alpha VOCs were notably higher as compared to the WT RBD.
The L452 and T478 residues may cause conformational change and result in new interactions in the mutant RBDs. The evaluation of MM/GBSA indicated a higher affinity of the RBD of the Delta VOC and ACE2 in comparison to the other VOCs. Mutations like T47K and L452R were found to increase the affinity of the RBD to the interfacial surface of ACE, which was considered to be responsible for the virulence of the Delta VOC and exhibited the strongest bond with ACE2.
On examining the ACE2 residues, it was observed that no Abs were associated with the D614, T478, and P681 residues in the mutated VOCs while the binding epitopes of the four examined mAbs did not contain E48, K417, N501, L452, and T478 mutation sites.
Conclusion
The study findings showed that in the SARS-CoV-2 Delta VOC, the Nb20 nanobody significantly neutralized the virulence of the VOC. At the same time, mutations like T478K and L452R enhanced the binding affinity of the Delta RBD with ACE2. Furthermore, P681R in the Delta VOC facilitated the identification of the RBD by proteases, thus improving viral entry in the human host. Overall, the study showed that specific and dynamic analysis of the emerging variants is crucial to assess the Ab response to the viruses.
Journal reference:
- Cheng, M.H., Krieger, J.M., Banerjee, A., Xiang, Y., Kaynak, B., Shi, Y., Arditi, M., Bahar, I., Impact of New Variants on SARS-CoV-2 Infectivity and Neutralization: A Molecular Assessment of the Alterations in the Spike-Host Protein Interactions, ISCIENCE (2022), doi: https://doi.org/10.1016/j.isci.2022.103939, https://www.sciencedirect.com/science/article/pii/S2589004222002097