In a recent study posted to the medRxiv* preprint server, researchers evaluated the immune responses induced by the messenger ribonucleic acid (mRNA)-based severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccination against SARS-CoV-2 variants of concern (VOCs) in multiple myeloma (MM) patients.
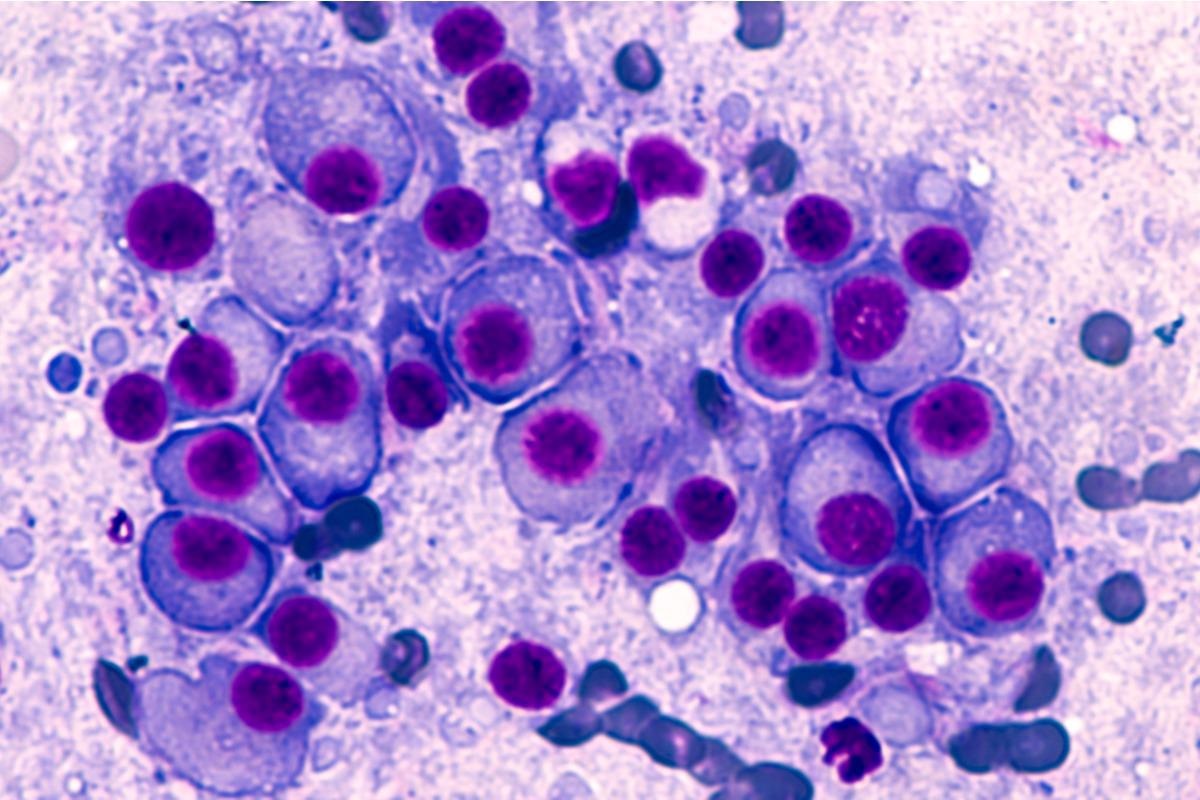 Study: Impact of Omicron variant on the response to SARS-CoV-2 mRNA Vaccination in multiple myeloma. Image Credit: David A Litman/Shutterstock
Study: Impact of Omicron variant on the response to SARS-CoV-2 mRNA Vaccination in multiple myeloma. Image Credit: David A Litman/Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
MM is a hematological malignancy marked by impaired cellular and humoral responses. Hence, the probability of viral and bacterial infections in these patients is high. MM patients demonstrate lower immune responses to vaccination because of their immunodeficient state. However, the cellular and humoral responses against the SARS-CoV-2 spikes (S) triggered by coronavirus disease 2019 (COVID-19) vaccination in MM patients and individuals with premalignant monoclonal gammopathies, like smoldering myeloma (SMM) and monoclonal gammopathies of undetermined significance (MGUS), are not yet understood.
About the study
In the present study, the researchers assessed the cellular and humoral immune responses to two doses of mRNA-based Pfizer (BNT162b2) vaccine and heterologous boost with Moderna (mRNA-1273) vaccine against SARS-CoV-2 Omicron, Gamma, Delta, Beta, and Alpha VOCs. The study was conducted in a cohort of 40 patients with MM, SMM, and MGUS in the Parma Hospital, in Italy from February 25 to July 23, 2021. The newly diagnosed MM (MMD) patients had received the first line of MM therapy, whereas MM patients with the relapsed-refractory disease (MMR) underwent the second-line therapy.
The peripheral blood (PB) samples were collected before the first dose of the Pfizer vaccine, 14±2 days after the second Pfizer vaccine dose, and 14±2 days following the booster vaccination with the Moderna vaccine. The team quantified SARS-CoV-2 S-specific CD4+ and CD8+ T cell responses among the MM, SMM, and MGUS patients.
Further, neutralizing antibody (NAb) titers and humoral responses like SARS-CoV-2 S immunoglobulin (IgG) Abs against vaccine homologous S and the Ss of the five SARS-CoV-2 VOCs among the study cohorts were also quantified. In a subset of 16 booster-vaccinated MM patients, including MMR and MMD, SARS-CoV-2 S-specific immune responses, specifically on the neutralizing capacity against the SARS-CoV-2 Ss, were analyzed.
Results
The results show that individuals with MMR developed lower neutralizing titers and S-specific Ab levels against SARS-CoV-2 following the two-dose Pfizer vaccination relative to SMM, MMD, and MGUS patients. All SARS-CoV-2 VOCs studied, mainly the Omicron variant, demonstrated substantial detrimental influence on the neutralizing capacity of vaccine-induced Abs in MMR, MMD, and SMM patients vaccinated with two doses of BNT162b2 vaccine. Nonetheless, no statistically significant relationship between humoral immunity and the age of the patients was observed.
In addition, MM patients had fewer S-specific tumor necrosing factor-α (TNF-α)- and interferon-γ (IFN-γ)-producing cytotoxic CD8+ T cells and S-specific interleukin-2 (IL-2)-producing CD4+ T cells than MGUS patients. The IL-2-producing CD4+ T cells were substantially lower in MMR, MMD, and SMM patients relative to the MGUS patients, whereas TNF-α- and IFN-γ-producing CD4+ T cells were comparable among these cohorts.
However, the mRNA-1273 booster vaccination enhanced the SARS-CoV-2 S-specific cellular and humoral immune responses in MMD patients and most individuals with MMR. The MMD patients exhibited a substantial increase in the NAb titers against almost all SARS-CoV-2 variants analyzed following the Moderna booster dose. In contrast, individuals with MMR had lower neutralizing capacity towards Omicron even after the heterologous booster vaccination, indicating this population was still prone to SARS-CoV-2 Omicron infection and clinically significant COVID-19.
Conclusions
According to the authors, this is the first study estimating the negative effect of the SARS-CoV-2 Omicron variant on the neutralizing capacity of the COVID-19 vaccine-induced antibodies in SMM and MM patients following two doses of mRNA-based SARS-CoV-2 vaccine. The study findings suggest that individuals with monoclonal gammopathies exhibit variable humoral and cellular immune responses to COVID-19 vaccination. Substantially lower immune responses were observed in MMR patients who received at least two lines of MM treatment relative to MGUS patients.
Furthermore, the heterologous SARS-CoV-2 mRNA booster vaccination with Moderna vaccine enhanced the humoral immunity against all SARS-CoV-2-Ss evaluated in the study among the MMD patients. Nevertheless, this effect was only partly observed in MMR patients, suggesting their risk of developing clinically relevant SARS-CoV-2 disease even after receiving a booster vaccination.
Collectively, the study emphasizes the significance of careful monitoring of three-dose vaccinated MM patients for COVID-19 in the light of heavily mutated variants like Omicron. Further, it highlights the need for SARS-CoV-2 preventive measures and devising additional prophylactic strategies like a fourth vaccine dose for MM patients, particularly those receiving several lines of MM therapy.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources