We had been developing EVs (including ASTEX) as therapies for inflammatory and fibrotic diseases. The potential applicability of the therapeutics inspired us to investigate their relevance to SARS-CoV-2 infection.
The ongoing pandemic has highlighted the need for researchers and organizations to come together to discover new solutions to tackle the virus. How important was it for you to get involved in the pandemic and what has this global collaboration shown to you as a researcher?
Indeed, it has; for us at the Smidt Heart Institute, we were very eager to get involved given the scale of the pandemic and the need to understand and address this complex disease. Given the versatile nature of translational research at Cedars-Sinai, we were able to quickly re-direct our efforts toward investigating the therapeutic relevance of ASTEX in SARS-CoV-2 infection.
Our work was a collaborative effort with colleagues at UCLA. This research, however, was more broadly enabled by the research that was done around the world investigating different facets of SARS-CoV-2 infection. It was truly inspiring to see the spirit of collaboration in the face of unprecedented challenges.

Image Credit: STILLFX/Shutterstock.com
Your “ASTEX” therapy consists of reengineered skin cells. Can you describe how you developed these cells and how they are able to repair heart tissue, lung tissue, and muscle damage in mice?
The development of ASTEX was a direct consequence of investigating the gene pathways necessary for cell therapy function. In our case, the cell therapy is called cardiosphere-derived cells; stromal cells from the heart that have a unique ability to repair injured tissue. These cells do so by secreting nanoparticles called extracellular vesicles (EVs for short) that contain bioactive molecules that trigger healing and repair.
Having discovered what the “special sauce” was we used this finding to activate these same pathways in an otherwise non-therapeutic cell type (skin fibroblasts), which are more readily available than heart cells. We found that when we genetically engineer these otherwise therapeutically inert skin cells with these genes, the fibroblasts began secreting EVs that were equally as therapeutic as the EVs from the original cardiac stromal cells.
When the COVID-19 pandemic hit, you applied your “ASTEX” therapy to see whether it could be a potential treatment for COVID-19. How did you adapt your therapy for this purpose and were there any hurdles you had to overcome when doing this?
This was the first time we had tested ASTEX in an infection model. One hurdle we had to circumvent was identifying the effective dose which is very different than the context of sterile injury.
What did you discover when applying your ASTEX therapy to SARS-CoV-2?
Much to our surprise, we found that ASTEX not only inhibited the inflammatory response, thereby protecting cells from the damaging effects of inflammation but also shut down the mechanism needed by the virus to hijack the cellular machinery for viral replication (a pathway called mTOR).
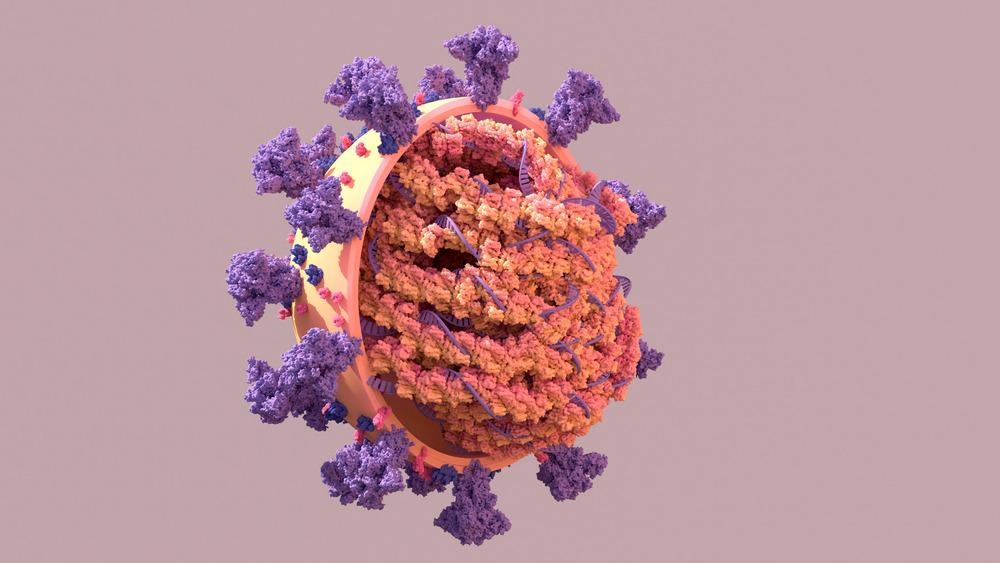
Image Credit: Design_Cells/Shutterstock.com
How does your new treatment differ from others that currently exist for COVID-19? Why is this important?
Unlike conventional therapy, it is combinatorial in nature and, therefore, addresses the natural redundancies that exist in a complex biological system. Conventional therapies target a limited number of targets whereas a complex biologic (like ASTEX) delivers a plethora of bioactive molecules that act on several levels of cell signaling which, from first principles, would be more effective.
Are you hopeful that with continued research into COVID-19, we will see more and more treatments becoming available?
“Hope springs eternal”; the dogged pursuit and focus (towards addressing COVID-19) I have seen from my group, my colleagues on campus, and those in academia and industry inspire much optimism. The extent of COVID’s effects are yet to be fully observed and understood. These trying realities only underscore the importance of this work.
What are the next steps for you and your research?
The observations we collected thus far were done in vitro or “cells in a dish” so we are in the very early preclinical phase of the work. The next step would be to test the ability of ASTEX in an animal model.
After this, we would follow the consistent path of any therapeutic towards translation, including work with the FDA to file the necessary applications and the planning and execution of clinical trials.
Where can readers find more information?
Readers can read more about this work from our initial publication that describes the development of ASTEX in our publication from 2019 (https://www.nature.com/articles/s41551-019-0448-6), our more recent publication of the application of ASTEX in pulmonary injury (https://pubmed.ncbi.nlm.nih.gov/34660588/) and our current publication describing its antiviral and cell-protective effects in the context of SARS-CoV-2 infection (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8841010/). For more general information, readers are welcome to review the original press release from the Cedars-Sinai Newsroom: https://www.cedars-sinai.org/newsroom/scientists-identify-possible-new-treatment-for-covid-19/
About Dr. Ahmed G. Ibrahim
My group at the Cedars-Sinai Smidt Heart Institute focuses on the development of extracellular vesicles, nano-sized lipid bilayer particles, and their molecular cargo for therapeutic application. I earned my PhD from the Cedars Sinai graduate program in Biomedical Sciences and Translational Medicine where I first discovered the role of EVs in cell therapy.
Since then I have worked to understand the mechanism by which EVs trigger healing in injured tissue and methods of engineering cells to produce therapeutically relevant EVs in a variety of disease contexts.