In a recent study posted to the medRxiv* preprint server, researchers evaluated the magnitude and durability of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike (S)-binding antibody titers mounted in response to SARS-CoV-2 infection in the pre-variant era, i.e., before August 2021 among healthcare workers (HCWs) of New York City (NYC).
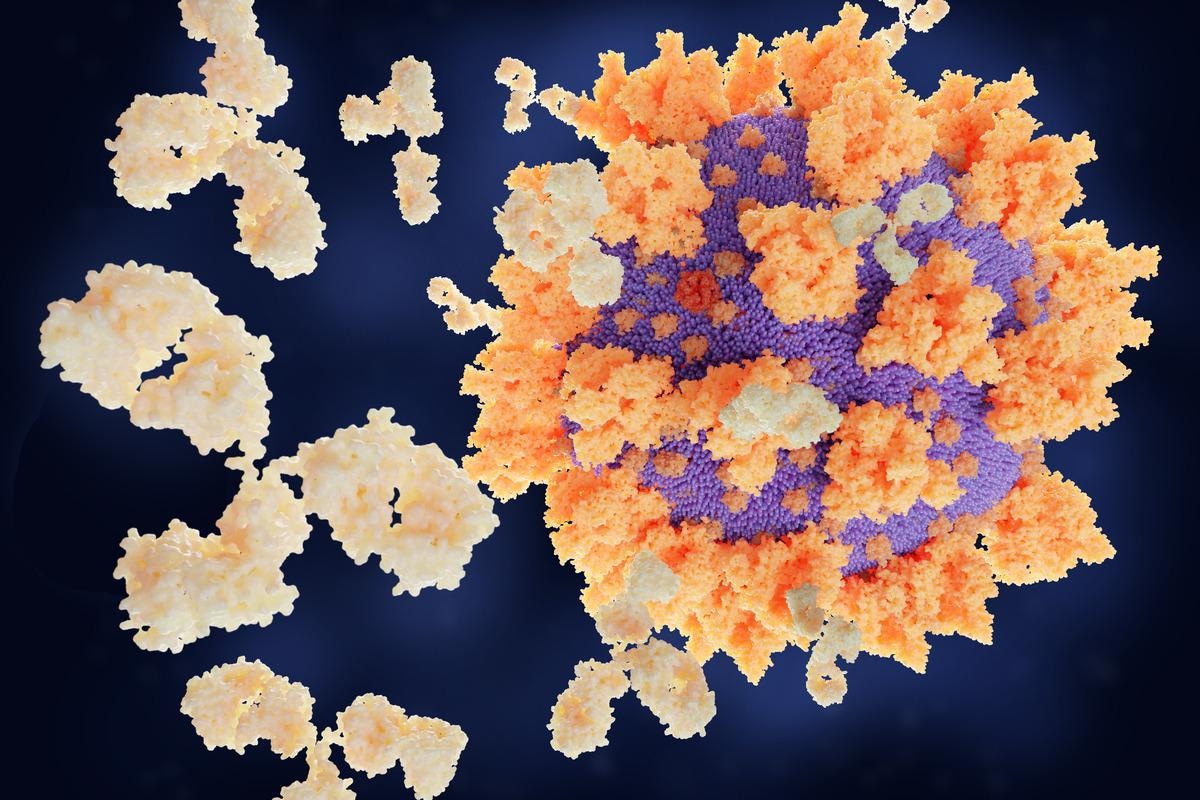 Study: SARS-CoV-2 spike-binding antibody longevity and protection from re-infection with antigenically similar SARS-CoV-2 variants. Image Credit: Juan Gaertner/Shutterstock
Study: SARS-CoV-2 spike-binding antibody longevity and protection from re-infection with antigenically similar SARS-CoV-2 variants. Image Credit: Juan Gaertner/Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Background
The first coronavirus disease 2019 (COVID-19) case was detected at the Mount Sinai Health System in NYC on February 29th, 2020, following which the initial COVID-19 wave overwhelmed the local health care systems. Due to the higher number of patients with severe COVID-19 manifestations, infection fatality rates reached as high as 1 and 1.5%.
The Protection Associated with Rapid Immunity to SARS-CoV-2 (PARIS) study enrolled HCWs with and without prior SARS-CoV-2 infection between April 2020 and August 2021 [before the emergence of SARS-CoV-2 variants of concern (VOC)]. As the COVID-19 pandemic continues, how antibodies are elicited in response to SARS-CoV-2 infection before the emergence of VOCs and how they offer protection against reinfection from antigenically similar variants has remained a topic of active interest.
About the study
In the present study, researchers analyzed sera samples of 400 participants of the PARIS study to evaluate the risk of SARS-CoV-2 infection and seroreversion for an average of 84 days. They collected samples from all the study participants every two to four weeks and analyzed data on SARS-CoV-2 exposure and clinical symptoms throughout the study period. The study covariates included gender, age, and baseline antibody titers (<1:800, ≥1:800).
The team could gather information regarding seropositivity for only 137 participants based on a positive SARS-CoV-2 nucleic acid amplification test (NAAT) or positive SARS-CoV-2 antibody test. Therefore, they could model the durability of SARS-CoV-2 S-binding immunoglobulin G (IgG) antibody using data of only these participants. The study modeled antibody titer variations over time, assuming that the antibodies wane at the same rate over time regardless of baseline titer, and its waning varies with the baseline titer. The team transformed S titers ranging from 1:80 to 1:6,400 to the log2 scale so that a one-unit increase reflected the doubling of IgG antibody titers.
Further, the researchers used a two-step enzyme-linked immunosorbent assay (ELISA) to screen sera samples at a single dilution (1:50) for IgG against the recombinant receptor-binding domain (RBD) of the SARS-CoV-2 S. Next, they detected antibodies against the full-length S protein and determined the end-point titers by serially diluting sera from 1:80 to 1:102,400.
Results
The study findings revealed that only 6% of the COVID-19 cases showed seroreversion with antibody levels waning below the detection level in the full-length S IgG binding antibody ELISA. Consistent with previous findings, the study participants 40 years or older had 1.6-fold higher antibody titers than the younger individuals. Contrasting to prior reports, the female participants had 1.4-fold higher antibody titers than the male participants.
The PARIS cohort had younger and overall healthy HCWs with mild infections. Presumably, sex-related variations would have become less apparent if severe COVID-19 manifestations, resulting in higher antibody levels, had been included in the analysis.
Intriguingly, although the magnitude of antibody responses varied with age and sex, the authors did not observe any sizable age- or sex-related differences in the kinetics of the antibody levels.
During the study period, ten naïve individuals contracted SARS-CoV-2 infection; additionally, one individual with low titers sero-reverted before reinfection and became SARS-CoV-2-infected. This suggested a significant role of S-binding antibody titers in offering protection from reinfection.
Conclusions
Previous studies reported that protection from reinfection ranges around 80-90% if the circulating SARS-CoV-2 variants are antigenically similar or homologous to variants that caused SARS-CoV-2 infections early in the pandemic.
The current study was conducted before the circulation of SARS-CoV-2 VOCs in NYC. Assuming that the study participants contracted SARS-CoV-2 infection from homologous strains, the study results might be undervaluing the immune protection based on the S-binding antibody titers against reinfection from antigenically distinct variants, such as Omicron. However, since the data collection was frequent (every two to four weeks), it allowed greater granularity while modeling the durability and effectiveness of SARS-CoV-2 antibody responses.
Accordingly, the overall estimates of antibody responses against SARS-CoV-2 infection showed an initial strong peak due to short-lived plasmablasts in the peripheral blood circulation, followed by a gradual decline and stabilization over follow-up months.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources