Using soluble spike (S) protein as bait, several separate investigations have isolated anti-severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) specific B cells from those infected or those who had received a coronavirus disease 2019 (COVID-19) vaccine. The neutralizing antibodies developed using this method almost always targeted the receptor-binding domain (RBD) and were generally more effective than those that targeted the N-terminal domain (NTD).
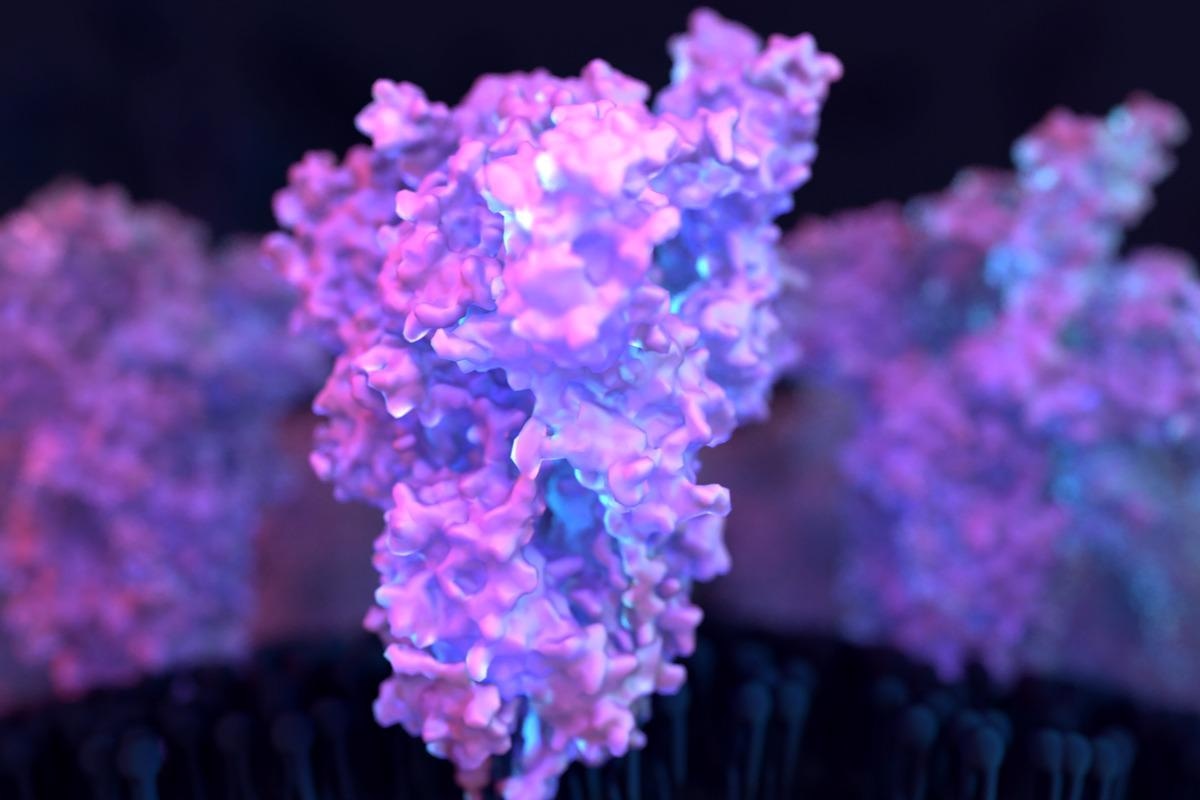 Study: Analysis Of Memory B Cells Identifies Conserved Neutralizing Epitopes On The N-Terminal Domain Of Variant SARS-Cov-2 Spike Proteins. Image Credit: Design_Cells/Shutterstock
Study: Analysis Of Memory B Cells Identifies Conserved Neutralizing Epitopes On The N-Terminal Domain Of Variant SARS-Cov-2 Spike Proteins. Image Credit: Design_Cells/Shutterstock
Background
Unlike RBD, anti-NTD neutralizing antibodies have predominantly targeted a single supersite with varying loops bordered by glycans. Several variants of concern have altered supersite residues, including Beta, Gamma, and Omicron. The latter has three deletions, four amino acid changes, and insertion in the NTD, rendering antibodies to the supersite inactive. The S protein of PMS20, an artificial construct strongly resistant to antibodies, has residues in this site mutated, and chimeric proteins made from wildtype (WT) and PMS20 proteins display NTD-specific antibodies are an essential element of the neutralizing action in convalescent and vaccine recipient plasma.
The study
In a recent study published in Immunity, a team of researchers evaluated the human antibody response to the NTD of the S protein by investigating a group of individuals who had previously been infected with SARS-CoV-2 or who had received an mRNA vaccine through the isolation of the NTD domain used as a probe to capture NTD-specific antibody-producing B cells.
Six individuals contributed 275 monoclonal antibodies (mAbs), with 103 neutralizing at least one of the three strains: Wuhan-Hu-1, Gamma, or PMS20. Six complementation groups were discovered based on competition binding assays among the 43 neutralizing antibodies that were subsequently described.
The researchers looked at a previously documented longitudinal cohort of patients sampled 1.3- and 12-months following infection, with some receiving an mRNA vaccination about 40 days prior to the study. ELISA was used to detect antibody responsiveness in plasma against the isolated Wuhan-Hu-1 and Omicron NTD. Anti-NTD Wuhan-Hu-1 or Omicron ELISA titers did not correlate with age, sex, symptom intensity, symptom duration, or time between the onset of symptoms and first visit to the clinic.
Anti-Wuhan-Hu-1 NTD IgG response was not changed substantially between the 1.3- and 12-month time intervals in previously infected patients who had not been immunized. On the other hand, IgG response to the Omicron NTD decreased considerably between the two time points. In previously infected patients who had not been vaccinated, there was no connection between NTD and RBD IgG ELISA response or NTD IgG ELISA responsiveness and plasma geometric mean half-maximal neutralizing titers. Vaccination of previously infected individuals increased IgG ELISA responsiveness to both Wuhan-Hu-1 and Omicron NTDs, with a positive connection between NTD and RBD ELISA. In all of the people studied, IgM and IgA anti-NTD response in plasma was weak, and only IgA was enhanced by vaccination.
To date, almost all anti-NTD antibodies have been produced by capturing specific memory B cells using the intact S protein. This mechanism of producing neutralizing anti-NTD antibodies only represents a small sub-group of the total anti-S antibodies that typically target a mutated single carbohydrate flanked epitope. To isolate memory B cells that produce antibodies specific for the NTD-domain, the researchers used a mixture of soluble Wuhan-Hu-1 and Gamma NTD proteins.
Between the 1.3- and 12-month time intervals, previously infected individuals who had not been vaccinated showed a minor but substantial drop in the number of anti-NTD memory B cells, which was increased by vaccination. Nine-hundred and fourteen anti-NTD antibody sequences were extracted from three previously infected vaccinated individuals and three non-vaccinated individuals and were assayed at two different time points. Different individuals developed closely related antibodies to NTD, similar to the anti-RBD response, with antibodies encoded by the genes VH1-24, VH3-30, VH3-33, VH4-4, and VH4-39 being over-represented.
The authors used biolayer interferometry tests to see if antibody affinity improved between the two time points. Among persisting clones and antibodies discovered only at one time point, affinity to the Wuhan-Hu-1 NTD improved between 1.3 and 12 months. Anti-NTD antibodies grow to higher affinity within the first 12 months after infection, regardless of later vaccination.
Implications
Infection from or vaccination derived from the Wuhan-Hu-1 strain results in relatively specific antibody responses to Wuhan-Hu-1, that are much less effective against subsequent variants such as Omicron. Memory B cell populations, on the other hand, are substantially varied in response to viral infection or vaccination to include high-affinity antibodies capable of neutralizing a wide range of variants. This varied group of memory B cells and their associated memory T cells are expected to play a key role in the typically milder course of infection in those previously infected with SARS-CoV-2 and/or those who have received the vaccine.