Additionally, they explored several microbiota-based therapeutic and prophylactic interventions for coronavirus disease 2019 (COVID-19) and post-acute COVID-19 syndrome (PACS).
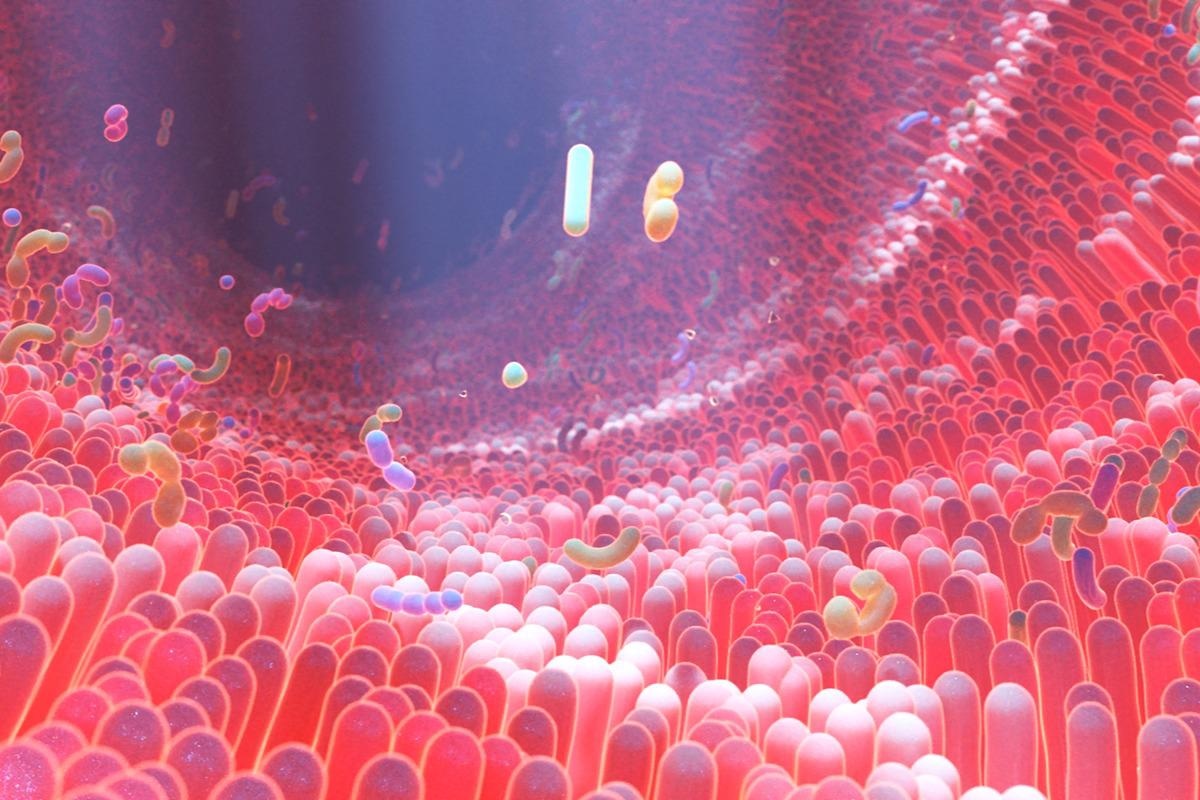 Study: Alterations in microbiota of patients with COVID-19: potential mechanisms and therapeutic interventions. Image Credit: Alpha Tauri 3D Graphics/Shutterstock
Study: Alterations in microbiota of patients with COVID-19: potential mechanisms and therapeutic interventions. Image Credit: Alpha Tauri 3D Graphics/Shutterstock
In humans, microbiota inhabits the respiratory and gastrointestinal tracts and serves multiple functions. They decompose carbohydrates and proteins, absorb nutrients, biosynthesize vitamins, and induce host immunity. However, they are also associated with several diseases and influence human health directly and indirectly.
Therefore, several reports have demonstrated that many COVID-19 patients present with respiratory and gastrointestinal manifestations, such as difficulty in breathing, diarrhea, nausea, and abdominal pain. Clinical evidence indicates that SARS-CoV-2 predisposes patients to secondary infections of the respiratory and gastrointestinal tracts leading to morbidity and even mortality in some cases.
Microbiota and their potential role in COVID-19
SARS-CoV-2 seizes host cell-surface transmembrane protease serine 2 (TMPRSS2) to activate its spike (S) protein, which, in turn, cleaves angiotensin-converting enzyme 2 (ACE2) receptors to facilitate viral binding and replication inside hosts. The human gastrointestinal and respiratory tracts are targets of SARS-CoV-2 invasion as they strongly express ACE2 and TMPRSS2. Moreover, they are inhabited by large microbial populations, which help regulate immune homeostasis and pathogenic infections.
Research has demonstrated that in a phenomenon termed colonization resistance, the symbiotic bacteria in the respiratory tract inhibit SARS-CoV-2 colonization of the mucosal surfaces to prevent infection.
Although aerosol droplets and fomite are the primary transmission routes of SARS-CoV-2, several recent studies have suggested that it also spreads through the oral-fecal route and infects the gastrointestinal tract. Accordingly, a population-based Chinese study showed that stool samples from ≤53% of COVID-19 patients were positive for SARS-CoV-2 viral ribonucleic acid (RNA), and their endoscopic examination revealed colon damage in some cases.
Microbiota-linked respiratory and gastrointestinal COVID-19 symptoms
The COVID-19 clinical manifestations vary greatly among affected individuals. Studies have reported shortness of breath in 53–80% of patients; likewise, people suffer from sputum production, dry cough, and sore throat. Although uncommon, 11–39% of all COVID-19 patients also suffer from gastrointestinal symptoms, including abdominal pain, vomiting, and diarrhea, associated with a heightened risk of hospitalization and greater disease severity.
An early Chinese study revealed that COVID-19 patients inhabited opportunistic pathogenic bacteria which disturbed their microbiota eubiosis. Accordingly, over 30% of critically ill COVID-19 patients had rhinovirus B and herpes alphavirus 1 infection. Additionally, their clinical sputum and nasal secretion cultures showed the presence of Burkholderia cepacia complex (BCC), Staphylococcus epidermidis, and Mycoplasma spp.
The researchers investigating the gut dysbiosis in COVID-19 patients found relatively lowered anti-inflammatory bacteria, namely, Roseburia, Eubacterium, Lachnospiraceae, and Faecalibacterium prausnitzii compared with the gut microbiomes of healthy individuals. The patients’ feces had several species of opportunistic bacteria, such as Clostridium hathewayi, Enterococcus, Enterobacteriaceae, Actinomyces viscosus, and Bacteroides nordii.
Another study observed opportunistic fungal pathogens in the feces of COVID-19 patients, including Candida albicans, C. auris, and Aspergillus flavus.
Gut dysbiosis persisted even after clearance of SARS-CoV-2 infection or disease recovery. Studies revealed different PACS symptoms related to different gut microbiota patterns and linkage of 81 bacteria with various PACS classes.
Microbiota-derived metabolites modulate lung antiviral immune responses
Gut microbiota metabolites, such as vitamins, carbohydrates, amino acid derivatives, and glycolipids, are small molecules produced from the bacterial metabolism of dietary substrates or directly from the bacteria. They are the key mediators of gut microbiota-host interactions that influence host immunity.
In the early stages of SARS-CoV-2 infection, mucosal-associated T cells (MAIT) respond to SARS-CoV-2 via restrictive major histocompatibility complex (MHC)-mediated recognition of riboflavin derivatives produced by gut microbiota. These bacteria include Bifidobacterium animalis, Bacteroides thetaiotaomicron, Lactobacillus casei, and Enterobacter cloacae. They are recruited by proinflammatory signals from the blood into the airways and participate in both local and systemic immune responses in the airways during the early stages of SARS-CoV-2 infection.
In another study, the researchers screened 84 microbe-associated metabolites and found that deaminotyrosine (DAT), a bacterial metabolite derived from flavonoids, significantly affected IFN signaling. Likewise, gut microbiota-derived lipopolysaccharides (LPS) also protected the lungs from viral infections.
Numerous studies have shown that various microbial metabolites are anti-inflammatory. For instance, in a study by Kim et al., they found that short-chain fatty acids (SCFAs) synthesized by several groups of gut microbiota promoted anti-SARS-CoV-2 antibody production in B cells to inhibit SARS-CoV-2 infection.
Microbiota-based therapies for COVID-19 prevention, prophylaxis, and treatment
Microbiota-based treatments, including fecal microbiota transplantation (FMT), probiotics, and prebiotics have shown clinical success in treating patients with diabetes, ulcerative colitis, and some viral infections. Similarly, gut commensals could modulate multiple host immunocyte subsets and mitigate SARS-CoV-2-induced inflammation.
Recent studies indicated the possibility of manipulating host gut microbiota to reduce SARS-CoV-2-induced inflammation and treat COVID-19-related complications. FMT could suppress COVID-19-induced cytokine storms and inflammation. Likewise, studies have demonstrated that supplementation with microbiota-targeted substrates (prebiotics) or one or several specific beneficial microbiota (probiotics) could modulate the gut microbiota favorably. This approach is relatively safer compared to FMT.
Similarly, engineering symbiotic bacteria with the ability to produce the desired metabolites and the capacity to target the correct locations in the host could help combat COVID-19. A Lactococcus lactis strain expressed and secreted anti-inflammatory cytokine interleukin 10 (IL-10) for colitis treatment. Similarly, engineered bacterial strains producing anti-inflammatory metabolites in the lungs and suppressing cytokine storms could emerge as a promising COVID-19 treatment.
Conclusions
There is adequate data evidence to show the role of microbiota in host immune responses to COVID-19. The age, sex, comorbidities, and external environmental factors, such as geographical location and season, influence the human microbiota composition. Moreover, it varies widely among individuals and populations.
Numerous clinical trials are currently evaluating the effectiveness of several microbiota-based treatments; however, none has published their results as yet. Additional clinical data is required to validate the safety and efficacy of microbiota-based therapies for COVID-19 or PACS patients.
The availability of more data on the associations between microbiota composition and susceptibility to coronaviruses could facilitate the designing of better prophylactics and therapies against the new SARS-CoV-2 strains. More importantly, more research is needed to determine how microbiota-based therapeutics could influence COVID-19 outcomes.