Individuals with MHCs might be at an elevated risk for severe outcomes of COVID-19 post-hospitalization. Most prior studies were limited by the small sample size or aggregation of MHCs concealing the risk differences. Moreover, earlier studies did not evaluate readmissions and hospital length of stay (LOS).
 Study: Mental Health Conditions and Severe COVID-19 Outcomes after Hospitalization, United States. Image Credit: lumezia.com / Shutterstock
Study: Mental Health Conditions and Severe COVID-19 Outcomes after Hospitalization, United States. Image Credit: lumezia.com / Shutterstock
About the study
In the current study, researchers investigated the associations of select MHCs with severe COVID-19 outcomes, LOS, and readmission. They analyzed a large United States (US)-based database of patient records. Patients hospitalized with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and discharged between March 1, 2020, and July 31, 2021, were identified. Anxiety, bipolar disorder, depression, and schizophrenia were select MHCs. The outcomes of interest were intensive care unit (ICU) admissions, LOS, invasive mechanical ventilation, all-cause readmission to the same hospital within 30 days, and all-cause mortality during the hospital stay.
The association between each MHC with each outcome was examined using mixed-effects models. The reference cohort comprised patients without the diagnosis of any MHC. Adjusted odds ratios and corresponding 95% confidence intervals (CIs) were estimated with logistic models. 95% CIs and percentage differences for LOS were computed using Poisson models. Models were adjusted for age, race, sex, ethnicity, admission month, insurance type, Elixhauser Comorbidity Index, and hospital characteristics.
Results
The study sample comprised 664,956 patients hospitalized with COVID-19. Most patients (77.1%) were 50 years or older, and 55% of male patients did not have any MHC diagnoses compared to 45% of females. More male patients (53.8%) than females (46.2%) had schizophrenia. In contrast, most female patients had depression (61.7%), anxiety (61%), or bipolar disorder (58.8%), outnumbering male patients.
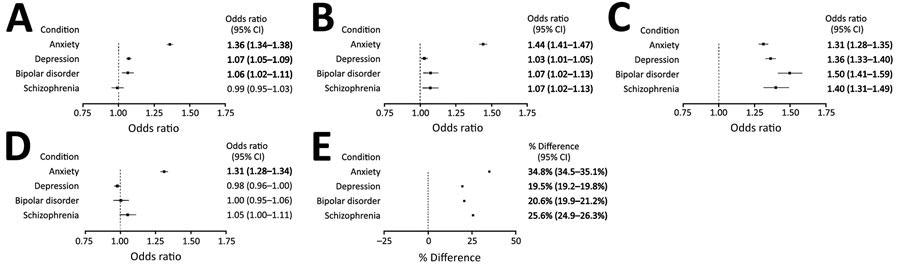
Outcomes of hospitalized COVID-19 patients (n = 664,956), by mental health condition diagnosis, compared with patients without mental health condition diagnoses in the Premier Healthcare Database Special COVID-19 Release, United States, March 2020–July 2021. For each condition, odds ratios represent the odds of the given outcome for patients with the condition compared with patients without mental health conditions. For length of stay, percentages represent the percentage difference in length of stay for patients with the condition compared with patients without mental health conditions. Covariates were selected based on factors known or plausibly associated with both the mental health condition and given outcome. Bolded values indicate statistical significance (2-sided α = 0.05), adjusted for multiple comparisons using the Bonferroni-Holm method.
Greater odds of ICU admission, mechanical ventilation, and death were noted for patients with anxiety than those without MHC. Patients with any of the select MHCs had significantly elevated odds of readmission. All select MHCs were significantly associated with longer mean LOS. Patients with anxiety, on average, had the longest hospital stay of 34.8 days, followed by those with schizophrenia (25.6 days), bipolar disorder (20.6 days), and depression (19.5 days).
Conclusions
The authors found that anxiety was strongly associated with severe disease outcomes. Each of the select MHCs was independently associated with an increased risk of all-cause readmission within 30 days and longer mean LOS. These results could not be compared with findings from previous studies because they had substantial heterogeneity in data/results, aggregation of MHCs, and populations with varying risk profiles, among others.
Moreover, earlier studies found no significant relationship between anxiety and increased risk for mechanical ventilation, ICU admission, or in-hospital mortality. In contrast, most others did not evaluate outcomes such as LOS and readmission. In summary, MHCs might aggravate respiratory diseases, increasing the risk for readmission or prolonged hospital stay in non-psychiatric hospitalizations. The study showed differences in the risks of each select MHC and provided evidence that MHCs could be deemed high-risk factors for COVID-19 patients.