A number of symptoms that individuals with COVID-19 may experience also occur among those without SARS-CoV-2 infection. Therefore, it is crucial to carefully investigate the extent and length of time of persistence of these symptoms following COVID-19 recovery.
 Study: Characterising patterns of COVID-19 and long COVID symptoms: Evidence from nine UK longitudinal studies. Image Credit: eamesBot / Shutterstock
Study: Characterising patterns of COVID-19 and long COVID symptoms: Evidence from nine UK longitudinal studies. Image Credit: eamesBot / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
About the study
In the present study, researchers collated electronic health records (EHR) data from the longitudinal health and wellbeing program of the UK National core studies between July 2020 and September 2021. Since EHRs poorly capture COVID-19 symptom persistence, they performed coordinated standardized analyses across nine longitudinal studies. The study approach minimized the heterogeneity of datasets of all the included studies and their designs besides maximizing comparability.
The team considered the 'no COVID-19' category as the reference group and the 'COVID-19 in last 12 weeks' category as the baseline group. The third study group was 'COVID-19 > last 12 weeks.' The researchers used a questionnaire to gather information regarding COVID-19 and its symptoms in all the study participants. The period of reporting of symptoms ranged between two weeks and two months in the included studies. In each study, participants reported the presence of symptoms, whether or not attributable to any specific cause. Further, for each study, the researchers conducted latent class analyses (LCAs) of reported symptoms separately within each COVID-19 status indicator category derived previously.
Furthermore, they used random-effects meta-analysis to combine prevalences of symptoms within the core symptom set across studies. They also combined odds ratio (ORs) for COVID-19 symptoms within the core symptom set across studies using the same analytical method.
Study findings
People in the baseline group exhibited the highest prevalence of known COVID-19 symptoms, including cough, fever, and loss of smell and taste. Since the study compared nine studies simultaneously, variations in the participants' age and geography varied the prevalence of some symptoms across studies. In other words, the current study results had face validity. Across all three study groups, the prevalence of runny nose and sneezing did not seem to vary, indicating these symptoms were not COVID-19-specific.
Using the symptom clustering analyses, the authors found a maximum of two symptom patterns among any of the COVID-19 groups. Some previous studies have also similarly found two symptom patterns. Caspersen et al. observed two distinct patterns of post-acute COVID-19 symptoms, viz., neurocognitive and cardiorespiratory. Likewise, Peluso et al. observed two clusters of patients, one with high symptom prevalence and the other low, with symptoms collated into seven domains. A higher symptom burden was more common among individuals with COVID-19 in the last 12 weeks than with no COVID-19.
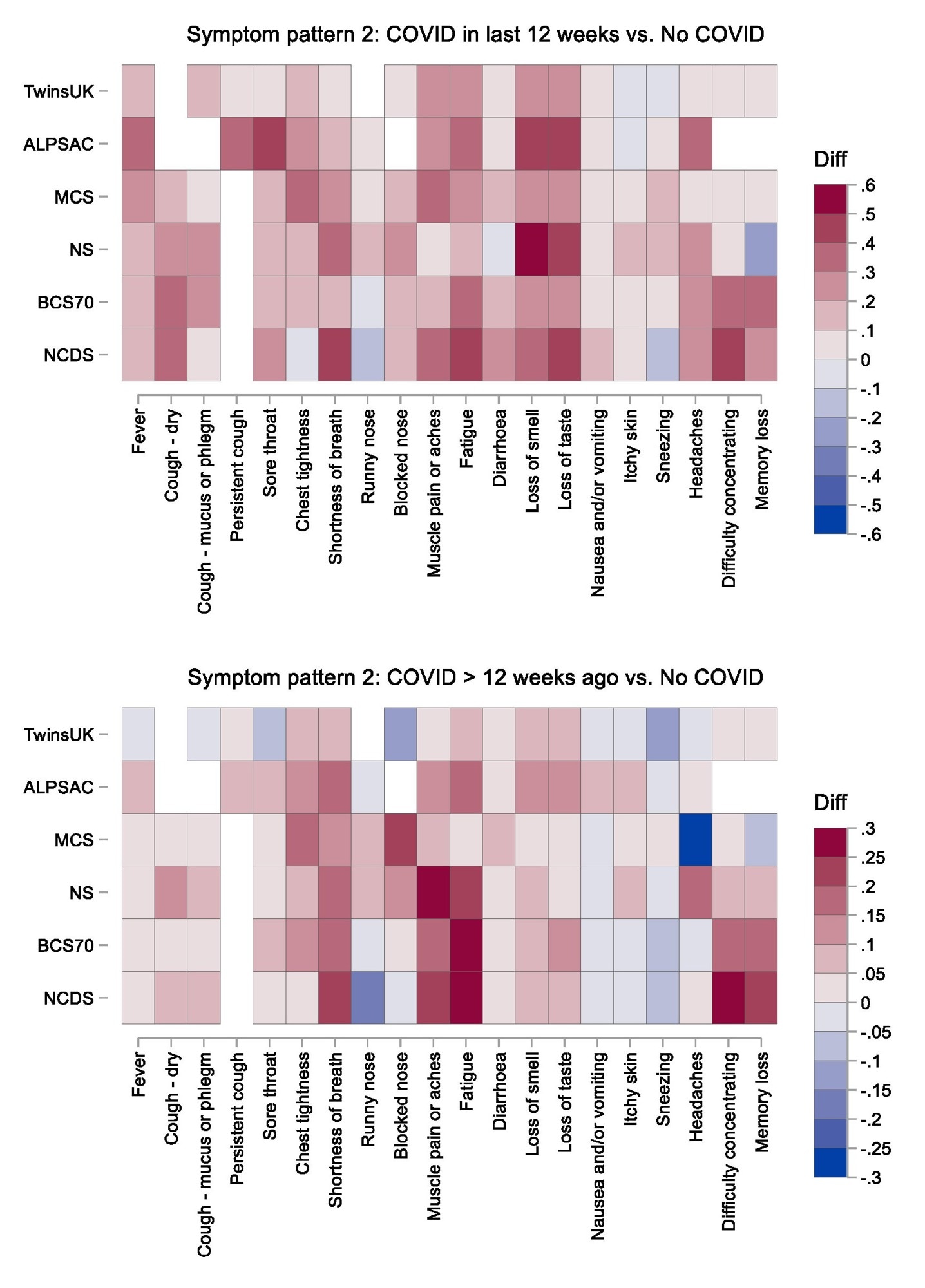
Heatmap of symptom probability differences comparing the two COVID-19 groups with the no COVID-19 group across all studies. NCDS: 1958 National Child Development Study; BCS1970: 1970 British Cohort Study; NS: Next Steps; MCS: Millennium Cohort Study; ALSPAC: Avon Longitudinal Study of Parents and Children. Notes: White cells indicate that the symptom was not asked about in in that study; ALSPAC results for “loss of smell or taste” are duplicated in the “loss of smell” and “loss of taste” cells; TwinsUK results for “confusion” are duplicated in the “difficulty concentrating” and “memory loss” cells.
While the symptom burden among those who never had COVID-19 was also substantially high, it was higher among those who have had COVID-19. This finding highlighted the importance of a control group in the analyses of COVID-19 symptoms. In fact, a lack of appropriate controls often hinders evaluating symptoms specific to acute COVID-19 and long COVID.
The authors compared the symptoms in COVID-19 in the last 12 weeks and no COVID-19 groups to find that their symptoms characterized acute COVID-19 and ongoing symptomatic COVID-19. These symptoms were fever, muscle pain, loss of taste and smell, dry cough, fatigue, shortness of breath, and breathing difficulty. Furthermore, symptoms identified by comparing the COVID-19 > last 12 weeks and no COVID-19 groups resembled the characteristic symptoms of long COVID. Consistent with existing literature, these symptoms were shortness of breath, impaired cognition, chest pain, and fatigue. Previous clinical reviews and meta-analyses have identified similar symptoms characterizing long COVID; however, these studies did not have an appropriate control group, such as a 'no COVID-19' group accounting for reference population symptoms.
The current study relied on its participants to report their COVID-19 symptoms. The authors found a higher symptom burden was more common in females across all three study groups. It was likely due to differential reporting of similar symptoms between males and females or females having a higher symptom burden.
Conclusions
The study discerned symptoms characteristic of acute COVID-19 and long COVID. However, the study results did not support the notion that long COVID might be a conglomerate of multiple syndromes discernible by differences in symptom patterns. In fact, all the identified symptoms largely replicated those previously identified in the literature.
Nevertheless, it is essential to build and expand the evidence base of typical long COVID symptoms to help its timely diagnosis and provide better treatment to patients suffering from long COVID.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Characterising patterns of COVID-19 and long COVID symptoms: Evidence from nine UK longitudinal studies, Ruth C E Bowyer, Charlotte Huggins, Renin Toms, Richard John Shaw, Bo Hou, Ellen J Thompson, Alex Siu Fung Kwong, Dylan M Williams, Milla Kibble, George B Ploubidis, Nicholas J Timpson, Jonathan A C Sterne, Nishi Chaturvedi, Claire J Steves, Kate Tilling, Richard J Silverwood, medRxiv pre-print 2022, DOI: https://doi.org/10.1101/2022.06.20.22275994, https://www.medrxiv.org/content/10.1101/2022.06.20.22275994v1
- Peer reviewed and published scientific report.
Bowyer, Ruth C. E., Charlotte Huggins, Renin Toms, Richard J. Shaw, Bo Hou, Ellen J. Thompson, Alex S. F. Kwong, et al. 2023. “Characterising Patterns of COVID-19 and Long COVID Symptoms: Evidence from Nine UK Longitudinal Studies.” European Journal of Epidemiology 38 (2): 199–210. https://doi.org/10.1007/s10654-022-00962-6. https://link.springer.com/article/10.1007/s10654-022-00962-6.