Additionally, the researchers studied the effect of 33 common point mutations using a custom bead-based 39-plex array. Specifically, they examined the effect on immunoglobulin G (IgG) recognition, fragment crystallizable gamma receptors (FcγRs)-engagement, and angiotensin-converting enzyme 2 (ACE2)-binding.
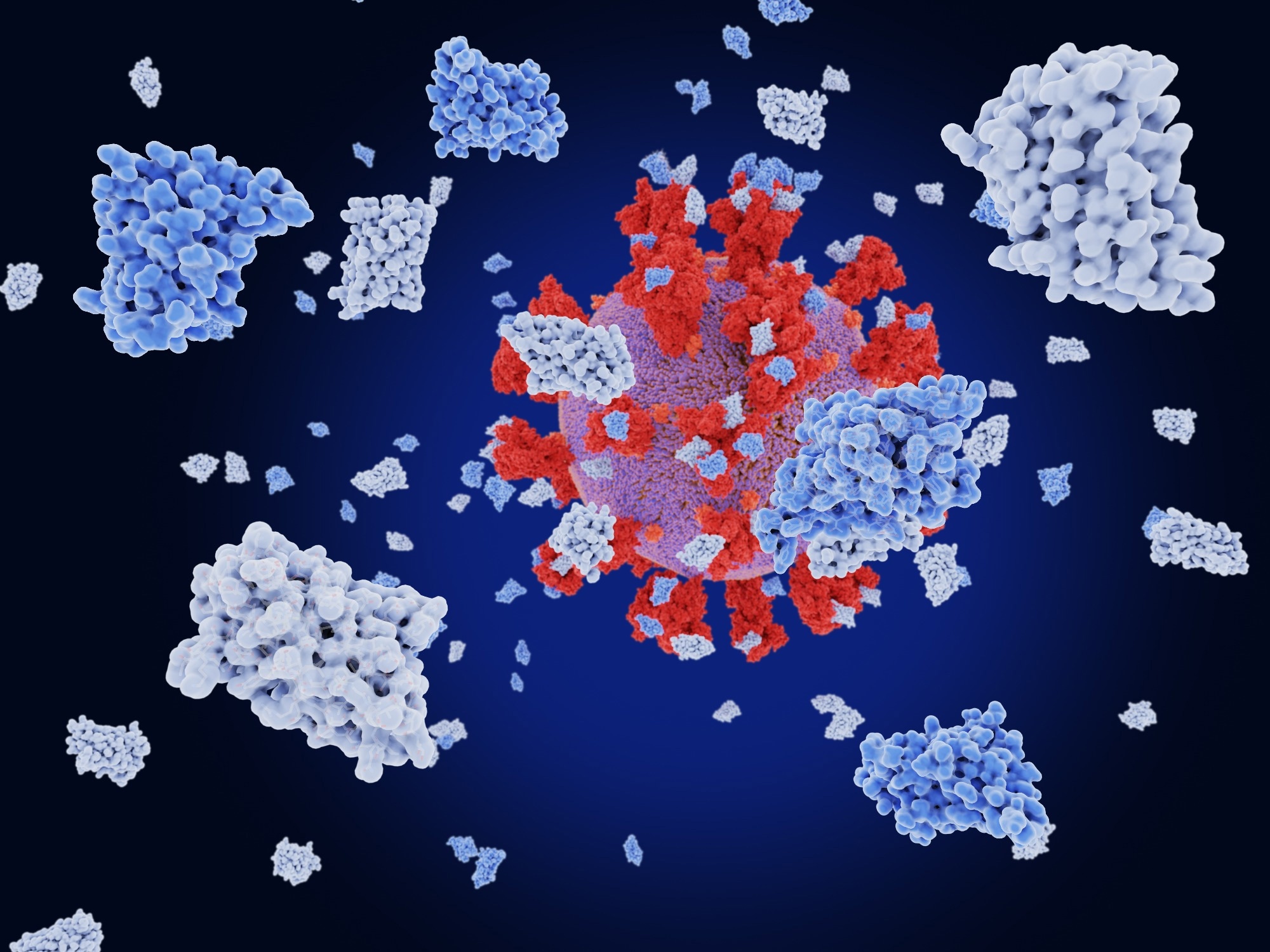 Study: Altered affinity to ACE2 and reduced Fc functional antibodies to SARS-CoV-2 RBD variants. Image Credit: Juan Gaertner / Shutterstock
Study: Altered affinity to ACE2 and reduced Fc functional antibodies to SARS-CoV-2 RBD variants. Image Credit: Juan Gaertner / Shutterstock

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Background
The RBD of the SARS-CoV-2 spike (S) protein is a mutation hotspot across all VOC lineages. The Beta and Omicron VOCs harbor RBD mutations such as N501Y, which enhance their ACE2 binding affinity and subsequently their infectivity and transmission potential. The RBD-targeting neutralizing antibodies (nAbs) induced following SARS-CoV-2 infection and coronavirus disease 2019 (COVID-19) vaccination block ACE2-binding on host cells, thus protecting them from symptomatic infection.
Some RBD mutations, such as E484K found in Beta and Gamma VOCs, result in a loss of epitope recognized by anti-SARS-CoV-2 nAbs, consequently reducing their neutralizing capacity. Likewise, Omicron BA.2 has 16 amino acid mutations at the RBD that facilitate evading neutralization. However, several antibodies directed towards the RBD also induce non-neutralizing activity.
Studies have barely investigated the impact of RBD mutations on the affinity to protein-altering ACE2 polymorphisms. Animal studies have demonstrated the importance of Fc-mediated immunity, where animals that received neutralizing monoclonal antibodies (mAbs) with compromised Fc-regions had higher viral burdens. Thus, a better understanding of antibody Fc effector functions, including antibody-dependent cellular phagocytosis (ADCP) and antibody-dependent cellular cytotoxicity (ADCC), could help improve protective signatures across all VOCs.
About the study
In the present study, researchers collected 16 IgG plasma antibodies samples from BNT162b2 vaccine recipients and 15 COVID-19 convalescent subjects. The convalescent study samples were collected between March and May 2020 when pre-VOC ancestral SARS-CoV-2 strains caused infections. They used a SARS-CoV-2 multiplex bead assay to measure antibody isotype and subclasses. Its results also indicated the capacity for antigen-specific antibodies to engage soluble FcγRIIa and FcγRIIIa-dimer constructs, a proxy readout for ADCP and ADCC activity, respectively.
The team used systems serology to observe the antibody repertoire of BNT162b2 vaccinees and convalescent subjects. Principal component analysis (PCA) showed that these subjects naturally separated into three groups based on the antibody signatures, with 15 antibody features contributing to observed differences between groups.
Further, the researchers used biolayer interferometry (BLI) to characterize the binding affinity of wild-type (WT)-ACE2 to VOC RBDs and a subset of single-point mutations. The BLI also helped the researchers assess the binding profiles of three low-frequency ACE2 polymorphisms, E35K, K26R, and S19P, to RBDs of Alpha, Beta, Delta, Gamma, Omicron BA.2 VOCs and ancestral strains RBD. It is noteworthy that ACE2 polymorphisms are present at a low frequency within the human population. For instance, S19P, predominant within African/African American populations, occurs at a low frequency of 0.3%.
Study findings
The current study had three key findings. First, the authors observed a loss of IgG recognition against the RBD of Omicron and Beta VOCs and numerous single-point mutations, including G446S and N501T. The ADCP assays validated that this reduced IgG recognition translated to a loss of FcγR-binding antibodies, which showed that RBD mutations in VOCs compromised Fc-effector functions. Overall, these results indicated evolutionary immune escape tendencies of Gamma, Beta, and Omicron VOCs.
Second, the researchers evidenced that the RBD-ACE2 affinity influenced the potential of antibodies to block ACE2-binding using a surrogate in-vitro neutralization assay. Third, the researchers used BLI to demonstrate that VOC mutations and human ACE2 polymorphisms, including E35K, K26R, and S19P, altered the RBD-ACE2 affinity and binding kinetics; which, in turn, influenced an individual’s susceptibility to SARS-CoV-2 infection.
Conclusions
The present study had a cohort of BNT162b2 individuals who received two vaccine doses. Now, most countries have expanded the currently approved vaccination regimen to three doses, which likely enhanced immune responses to VOCs. Future studies should dissect the impact of particular mutations on enhanced RBD-specific antibody responses.
Future studies should also explore how the current study findings would translate to other SARS-CoV-2 vaccines with more or less potent responses, such as messenger ribonucleic acid (mRNA)-1273. To conclude, all the VOC mutations, including common point mutations, RBD mutations, and their combination, had significant effects on RBD-ACE2 affinity, IgG-binding, and the Fc effector functions. Indeed, these sites are crucial for SARS-CoV-2 evolution and need continuous monitoring.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Journal reference:
- Preliminary scientific report.
Altered affinity to ACE2 and reduced Fc functional antibodies to SARS-CoV-2 RBD variants, Ebene R Haycroft, Samantha K Davis, Pradhipa Ramanathan, Ester Lopez, Ruth A Purcell, Li Lynn Tan, Phillip Pymm, Bruce D Wines, P Mark Hogarth, Adam K Wheatley, Jennifer A Juno, Samuel Redmond, Nicholas A Gheradin, Dale Godfrey, Wai-Hong Tham, Kevin John Selva, Stephen Kent, Amy W Chung, medRxiv pre-print 2022, DOI: https://doi.org/10.1101/2022.07.07.22277364, https://www.medrxiv.org/content/10.1101/2022.07.07.22277364v1