The first case of the human monkeypox virus (hMPXV) was confirmed by the United Kingdom Health Security Agency (UKHSA) in an individual traveling back from Nigeria on 7th May 2022. This patient developed rashes a few days before traveling to the UK, while hospitalization took place on his arrival to the UK. hMPXV was confirmed with the help of a reverse transcriptase polymerase chain reaction (RT-PCR) using a vesicular swab sample. Following this, more than 1,500 cases were suspected or confirmed in 45 countries, causing the World Health Organization (WHO) to call an emergency meeting to curb the virus's rapid spread.
MPXV is a double-stranded DNA virus that belongs to the Orthopoxvirus genus and Poxviridae family. It is a zoonotic virus present on WHO's list of viruses possessing pandemic or epidemic potential. It is a 200 to 250 nm large, enveloped, cytoplasmic virus that can enter the host cell through binding to glycosaminoglycans. However, limited studies are available on the origin of hMPXV, pathogenesis, and treatment.
A new review in the Virus Research journal aims to provide an overview of the recent advances reported concerning hMPXV virology.
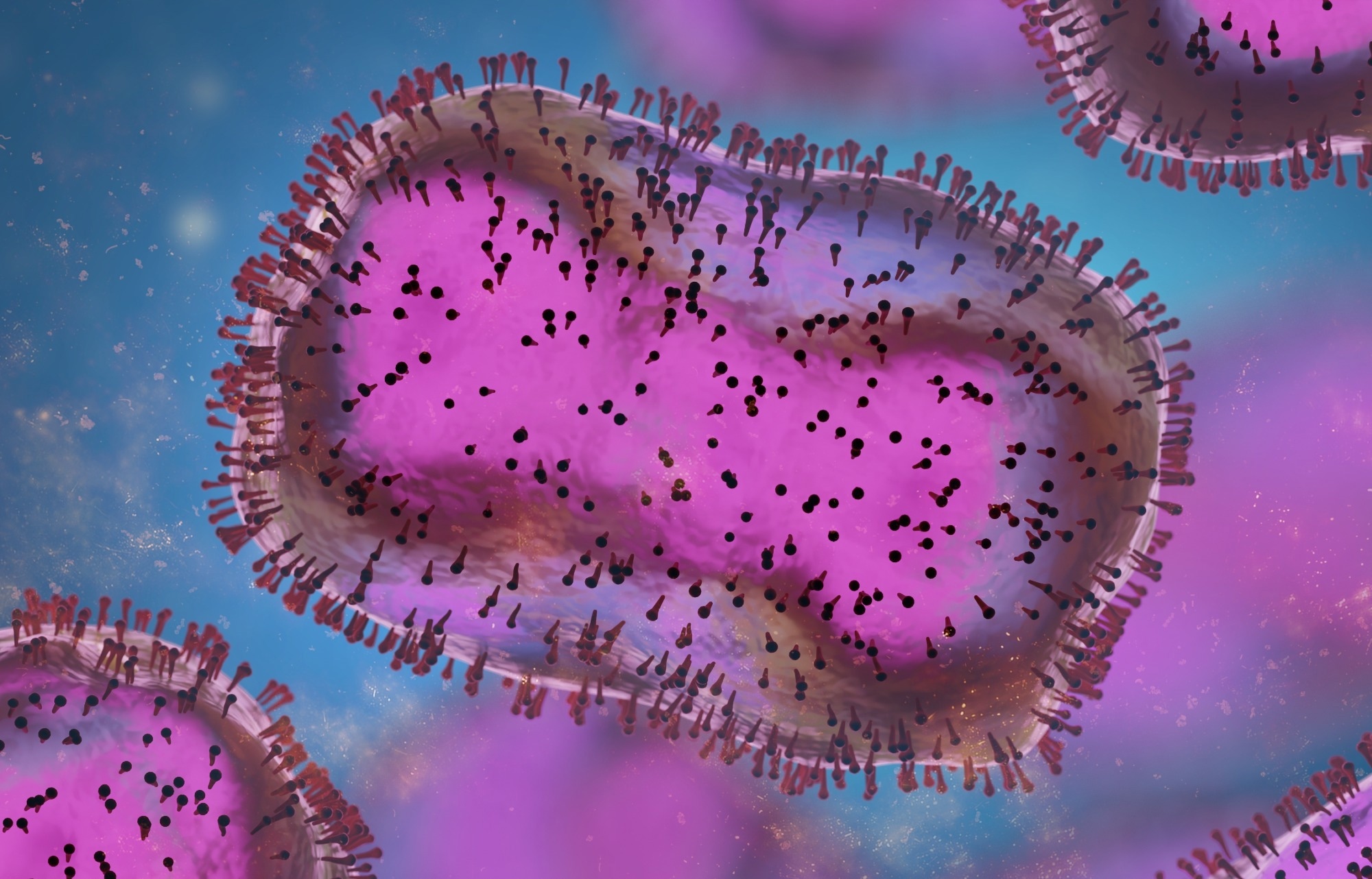 Review: The Virology of Human Monkeypox Virus (hMPXV): A Brief Overview. Image Credit: Dotted Yeti / Shutterstock
Review: The Virology of Human Monkeypox Virus (hMPXV): A Brief Overview. Image Credit: Dotted Yeti / Shutterstock
Origin of the virus
The first isolation of the virus took place from smallpox-like vesiculopustular lesions that appeared on imported monkeys in Denmark. For the next few years, similar outbreaks in monkeys were observed elsewhere. A widespread outbreak took place at a zoo in Rotterdam in 1966. Assumptions were made that the virus first affected South American giant anteaters before spreading to different apes and monkeys. Initial human infections were identified in individuals from Liberia and the Democratic Republic of Congo in 1970, which confirmed hMPXV as a distinct virus.
After that, the virus was found to be endemic to western and central African counties from 1970 to 2003. The first report of an outbreak outside Africa was reported in the United States during the import of nine different mammalian species from Ghana in 2003. A spill-over event was identified when a 3-year-old girl was brought to the emergency following a prairie dog bite. Following this, sporadic outbreaks have been observed worldwide that can be traceable to the endemic regions of Africa. However, accurate detection of its natural reservoir is still under investigation.
MPXV clades
The Orthopoxvirus is genetically and antigenically similar and comprises open reading frames (ORFs) with more than 90% sequence similarity among its members. Evolutionary changes in the virus are reported to be due to gene loss at the terminal ends of the genome and variations in gene copy number. The hMPXV genome size is approximately 197 kb and comprises about 190 non-overlapping ORFs along with a central coding region sequence (CRS) whose ends are flanked by inverted terminal repeats (ITRs).
The most described hMPXV clades are the West African (WA) and Central African/Congo Basin (CA) clades. The WA clade is found to cause milder infections with lower mortality rates, while the CA clade is found to cause more severe infections with a mortality of 10% among non-vaccinated people. Previous studies have indicated that the CA clade comprises 173 unique functional genes while the WA clade comprises 171. Moreover, 53 of the 56 virulence genes were observed in both clades. The virulence difference between both the clades was observed due to differences in COP-C3L, BR-209, and BR-203 gene orthologs. Additionally, the D14R gene was found to be another crucial anti-inflammatory factor that was absent from the WA clade and also contributed to the difference in virulence.
A recent analysis of the hMPXV genome from the 2022 outbreak indicated mutations of bases Cytosine (C) to Thymine (T) and Guanine (G) to Adenine (A) that might be caused by enzyme APOBEC3. Also, a 30-T base long sequence has been observed in the middle of the genome from the 2022 isolates, whose role is yet to be determined.
Pathogenesis
hMPXV pathogenesis included the entry of the virus, fusion, replication, and release. Two infectious forms of the virus have been observed to be produced, intracellular mature virions (MV) and extracellular enveloped virions (EV). MVs are found to be single membrane-bound, while EVs comprise a distinct triple membrane. Antibodies and vaccines that are unable to target and produce EV antigens are found to provide lower protection.
Furthermore, two multi-subunit complexes have been identified that are important for the completion of the viral infectious cycle, the Conserved Oligomeric Golgi (COG) and Golgi-Associated Retrograde Protein (GARP) complex. The GARP complex helps retrograde endosomal transport and comprises four vacuolar protein sorting (VPS) genes. The COG complex help in the maintenance of Golgi structure and intra-Golgi traffic regulation. It comprises two lobes, each consisting of 4 associated subunits.
Through bioinformatic analysis, the identification of two distinct regions, ORF 17 to 32 (R1) and ORF 179 to 193 (R2). Deletion of one or both regions has been found to reduce mice morbidity and mortality as well as attenuate viral replication. Additionally, hMPXV has been observed to upregulate core histones and downregulate histone expression regulation factors and cell membrane ion channels associated with the host cell cycle.
Cytokine storm
Similar to COVID-19, a cytokine storm was observed in the case of hMPXV infection that led to high levels of interleukins IL-4, -5, -6, and -10 and low levels of tumor necrosis factor-alpha, interferon alpha, and gamma, along with IL-2 and -12. hMPXV infections also induced a cascade of complementary B cell responses. In addition, six monoclonal antibodies were identified that targeted A33, B5, L1, D8, H3, and A27, which protected against orthopoxviral respiratory tract infection and systemic infection.
Diagnostic Modalities for hMPXV
Diagnosis of hMPXV can occur through viral culture and isolation, PCR, IgM/IgG serology testing, immunohistochemistry of specific antigens, and negative staining electron microscopy of the rash. Moreover, a sensitive diagnostic tool known as Antibody Immuno Column for Analytical Processes (AICAP) immunofiltration tool has been developed to detect all zoonotic orthopoxviruses. Recently, a recombinase polymerase amplification (RPA) assay has been developed that can detect the G2R gene of the virus in under 7 minutes. Metabolic activity, along with lymph node size, can also determine the presence of hMPXV infections. Also, positron emission tomography/computed tomography (PET/CT) imaging with [18F]-fluorodeoxyglucose (FDG) has been found to accurately predict the course of hMPXV disease for non-human primate models.
Treatment and Prophylaxis
Antiviral treatment with cidofovir or some other associated acyclic nucleoside phosphonate analog has been observed to be more effective in treating lethal hMPXV in monkeys post-24 hours of exposure as compared to smallpox vaccination. However, a new antiviral known as PAV-164 has been developed to inhibit MPXV replication and overcome resistance to available antivirals. Revesterol, a natural polyphenol, has also been found to reduce in vitro hMPXV replication against both clades significantly.
The Advisory Committee on Immunization Practices (ACIP) has recommended using the JYNNEOS vaccine as an alternative to the ACAM2000 vaccine in 2022. JYNNEOS has been developed from a replication-deficient modified vaccinia virus Ankara (MVA) and can be administered in a 2-dose regimen with 28 days between the doses. People with contact with more virulent orthopoxviruses are recommended to take a booster dose every two years, while those with contact with low virulent orthopoxviruses are advised to take a booster dose every ten years.
Recently, a DNA vaccine known as 4pox has also been developed to inhibit viral shedding and prevent the adverse impact of infection. In addition, recombinant vaccinia virus immunoglobulin (rVIG) and two human-chimeric monoclonal antibodies, c8A and c7D11, have also been found to be effective against MPXV. Moreover, CRISPR/Cas9-based targeted antivirals have also been observed to reduce orthopoxvirus viral titer by approximately 90%. With the onset of ring vaccination in countries such as the UK, the US, and Canada, it is vital to develop safer, more potent, and easy-to-distribute vaccines that can reduce the severity and prevent hMPXV infections.
The 2022 outbreak
The 2022 global outbreak is interesting since it lacks links to western or central Africa. Moreover, the transmission of the virus mainly among men who have sex with men (MSM) community is quite intriguing. The WA clade has been associated with the 2022 outbreak known to cause mild infections and less transmission among humans. The increase in human-animal interactions and climate change are suggested to accelerate zoonotic spill-over events. Epidemiological institutions and public health officials must be conscious and alert to detect future zoonotic infections, provide treatment options, and guide the general population.
Conclusion
The human monkeypox virus is a neglected zoonotic pathogen detected many years ago. However, the recent 2022 outbreak highlights the need for constant monitoring of the virus and the development of new and effective therapies. In addition, further research must be done to manage and contain the rapid spread of hMPXV across the globe.