One commonly reported symptom of COVID-19 and post-acute sequelae of COVID-19 (PASC) is anosmia or the loss of olfactory senses. Anosmia is thought to be caused by the effect of SARS-CoV-2 on the olfactory epithelium, which consists of the odor-detecting primary olfactory sensory neurons, a sustentacular cell layer forming a barrier, and basal stem cells or progenitor cells that restore the olfactory epithelium. Autopsy studies in humans and animal models have suggested various mechanisms explaining anosmia in COVID-19 patients, including gene expression changes in olfactory neurons, changes in the mucus layer around ciliated neuronal cells, altered gene expression in sustentacular cells, and inflammation.
However, the mechanisms behind persistent anomia in PASC patients are still unclear. Possible explanations include severe epithelial damage, neuroinflammation, and damage to the brain's olfactory bulbs or olfactory cortex. While autopsy studies on PASC patients have found persistent infections in the sustentacular cells and molecular changes in the sensory neurons, the epithelial anatomy has been found intact with no infection in the olfactory neurons.
About the study
In the present study, the researchers used biopsy samples of olfactory epithelium obtained from nine PASC patients experiencing persistent anosmia, which was verified using a smell identification test before the biopsy. Olfactory biopsy and mucus samples from normosmic individuals with and without a history of COVID-19 were used as control.
The biopsy samples were processed for single-cell ribonucleic acid sequencing (sc-RNA seq) to determine cellular or transcriptional alterations associated with the persistent olfactory dysfunction observed in PASC patients. In addition, immunohistochemical analysis was performed on the tissues using primary antibodies against a wide range of antigens comprising tubulin, cluster of differentiation (CD) 45, CD3, CD68, CD207, T-cell receptor gamma/delta (TCR γ/δ), the sustentacular cell-specific marker Ermin (ERMN), olfactory marker protein (OMP), SARS-CoV-2 nucleocapsid protein, and sex-determining region Y box 2 (SOX2).
Additionally, the mucosal samples were subjected to a fluorescent bead-based multiplex assay and flow cytometry to test for 13 chemokines and cytokines.
Results
The results reported infiltration of the olfactory epithelium with T cells secreting interferon-γ (IFN-γ) and changes in the population of myeloid cells resulting in an increase in CD207+ dendritic cells and a decrease in anti-inflammatory macrophages. Furthermore, gene expression analysis revealed responses to continued inflammatory signaling in the sustentacular cells despite the absence of SARS-CoV-2 proteins or ribonucleic acid (RNA). Compared to the number of sustentacular cells in the olfactory epithelium, the number of olfactory sensory neurons, especially mature neurons presenting OMP, was observed to be lower.
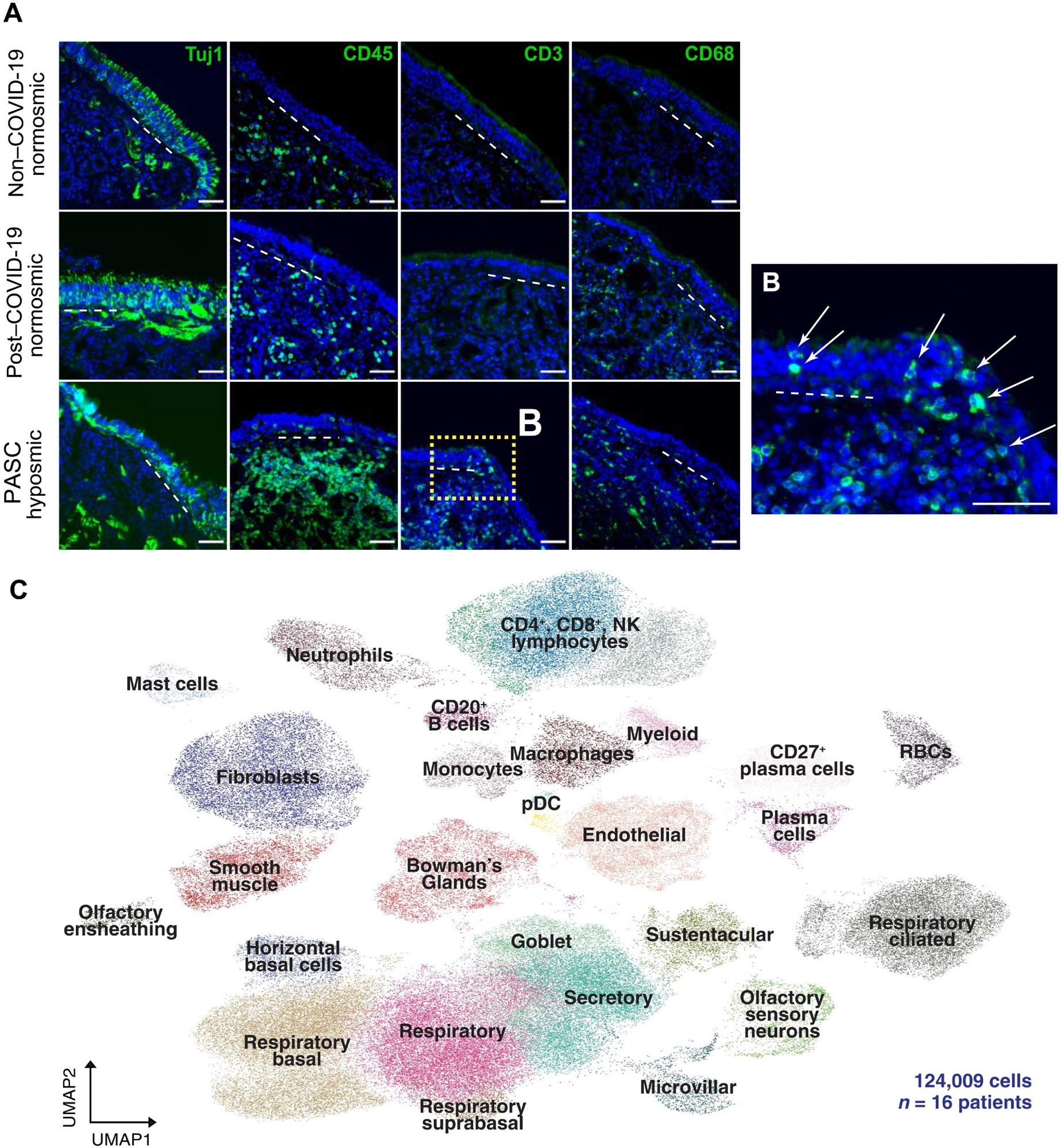
T cell infiltrates in nasal olfactory epithelial biopsies from PASC hyposmic patients. (A) Representative immunohistochemistry images of nasal biopsy tissue from normosmic non–COVID-19, normosmic post–COVID-19, or PASC hyposmic individuals. Tissue sections were immunostained for the TUJ1 neuronal marker, CD45 pan-immune cell marker, CD3 T cell marker, and CD68 myeloid cell marker. PASC hyposmic tissue showed dense CD45+ immune cell infiltration, including prominent CD3+ lymphocytic infiltration, which was absent in the normosmic groups; scattered CD68+ cells were present in all conditions. (B) The enlarged area (yellow box) from (A) shows CD3+ lymphocytes with prominent infiltration into the olfactory epithelium (white arrows); the dashed white line marks the basal lamina. Scale bar, 50 μm. (C) Additional nasal biopsies were processed for scRNA-seq to permit quantitative analyses. Uniform manifold approximation projection (UMAP) visualization of combined PASC hyposmic and control normosmic scRNA-seq datasets integrating 16 human nasal biopsies permitted robust cell cluster analysis and annotation. RBCs, red blood cells; pDC, plasmacytoid DCs.
In contrast to acute COVID-19 cases, there was an absence of transcriptomic changes in the olfactory sensory neurons, and severe inflammation was also not observed in PASC-related anosmic patients. Instead, interferon response signatures and lymphocyte populations expressing T-cell γ/δ and IFN-γ were observed in the olfactory epithelium samples of PASC patients with anosmia.
Comparison of immune cell phenotypes of humans with anosmia during PASC and those from hamsters with acute SARS-CoV-2 infections revealed that infiltrates in the olfactory epithelia of infected hamsters contained monocytes, neutrophils, and macrophages in the first week following infection, which were resolved by week two. In contrast, the olfactory epithelia of anosmic PASC patients were infiltrated with T cells for months following COVID-19. These differences indicated that the immunological responses during PASC-related hyposmia or anosmia differ significantly from the immunological responses during acute SARS-CoV-2 infections.
While the mechanisms behind the sensory dysfunction affecting olfactory sensory neurons, sustentacular cells, horizontal basal cells, and immune cells remain unclear, macrophage analysis in patients with severe COVID-19 has indicated that a proinflammatory reprogramming during acute SARS-CoV-2 infections induces long-term changes in other immune cell functions.
The results provide a potential for developing therapeutic options that can be topically delivered to the olfactory epithelium or olfactory cleft, which would also help avoid other systemic reactions to the therapies.
Conclusions
To summarize, the study examined olfactory epithelium biopsy samples from anosmic PASC patients using immunohistochemical analyses and sc-RNA sequencing. The results revealed significant differences between the immunological responses during acute SARS-CoV-2 infections and PASC-related anosmia. In addition, the olfactory epithelia in anosmic PASC patients were infiltrated with IFN-γ secreting T-cells, and gene expression indicated continued inflammatory signaling despite the absence of SARS-CoV-2 proteins or RNA in olfactory tissue.
Journal reference:
- Finlay, J. B., Brann, D. H., Abi Hachem, R., Jang, D. W., Oliva, A. D., Ko, T., Gupta, R., Wellford, S. A., Moseman, E. A., Jang, S. S., Yan, C. H., Matsunami, H., Tsukahara, T., Datta, S. R., & Goldstein, B. J. (2022). Persistent post–COVID-19 smell loss is associated with immune cell infiltration and altered gene expression in olfactory epithelium. Science Translational Medicine, 14(676). https://doi.org/10.1126/scitranslmed.add0484