The advent of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has renewed interest in these molecules 100 years after their discovery. During the coronavirus disease 2019 (COVID-19) pandemic, an acute-phase protein, C-reactive protein (CRP), served as a valuable diagnostic tool and prognostic indicator.
This liver-secreted acute-phase protein in humans increases by as much as 1,000 times in plasma in response to interleukin-6 (IL-6), a potent inducer of the transition from acute to chronic inflammation through reorientation of metabolic functions (e.g., decrease in albumin production).
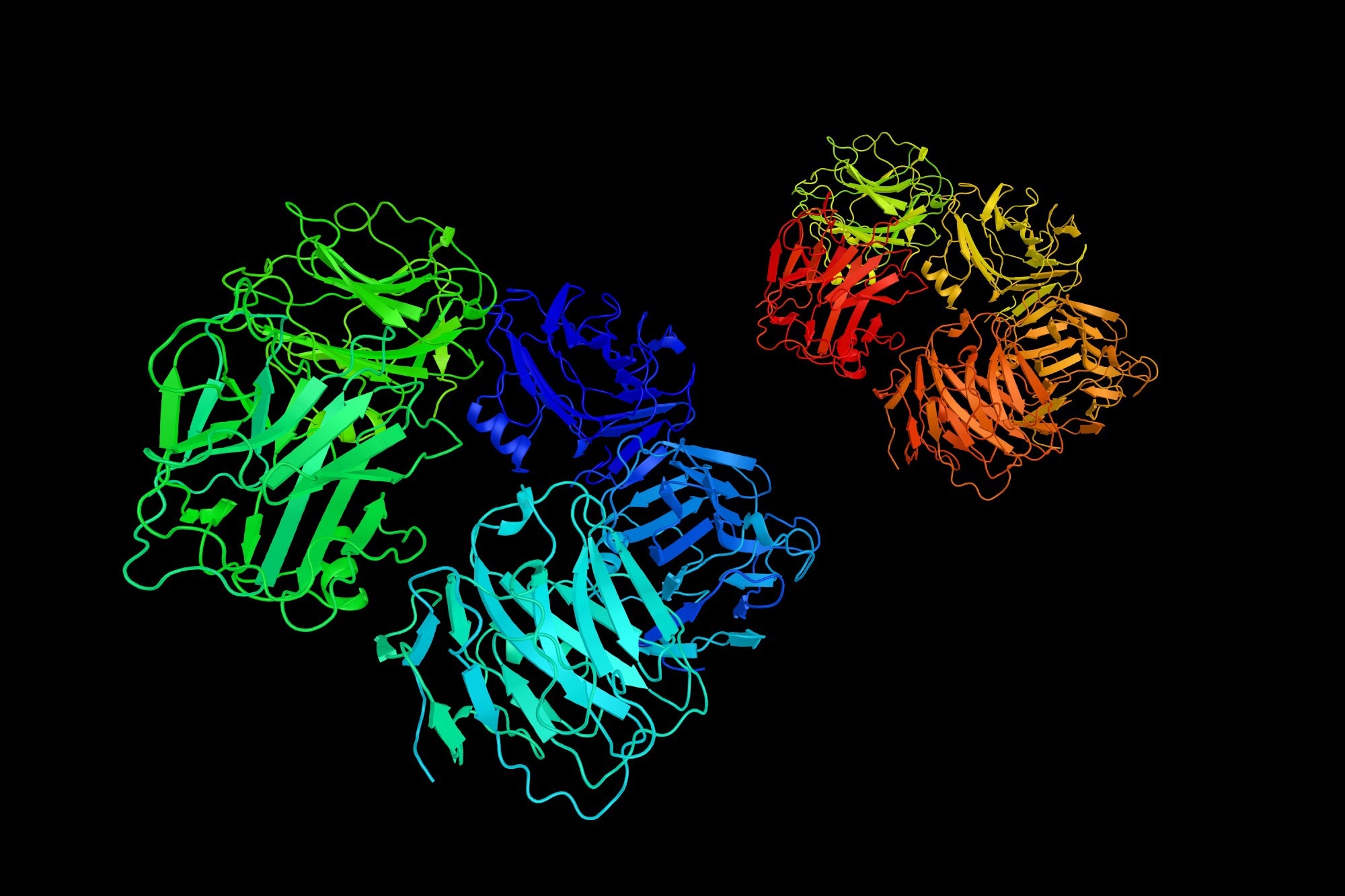 Review: Humoral Innate Immunity and Acute-Phase Proteins. Image Credit: ibreakstock / Shutterstock
Review: Humoral Innate Immunity and Acute-Phase Proteins. Image Credit: ibreakstock / Shutterstock
Origin of acute-phase proteins and associated acute-phase response
It is common knowledge that 'inflammation' encompasses diverse tissue reactions that magnify innate immunity and tissue repair, leading to the re-establishment of homeostasis. Studies have recently recognized the role of diabetes, obesity, and other metabolic dysregulations in eliciting inflammatory reactions.
Acute-phase protein levels increase in blood and other body fluids in response to local or systemic inflammation, referred to as the acute-phase response, wherein decreased albumin production, reoriented iron metabolism, altered leukocyte counts, and hormonal changes accompany this complex phenomenon.
The liver primarily secretes acute-phase proteins of approximately 200 types, mainly by hepatocytes and some other cell types (e.g., endothelial cells and tissue-resident macrophages, such as Kupffer cells). These cells are also the sources of cytokines that activate hepatocytes to synthesize acute-phase proteins.
These non-hepatic sources also secrete some acute-phase proteins upon stimulation by microbes, e.g., pentraxin 3 (PTX3). Locally, adipocytes also elevate the systemic concentration of acute-phase proteins, such as serum amyloid A3 (SAA3), in response to IL-1 and IL-6. Adipocytes also express vast quantities of complement factors (C3, D, and B).
The molecules constituting the humoral arm of innate immunity, such as pentraxins and ficolins, act as ante-antibodies by initiating complement activation. These help clear pathogens and dead cells by opsonization, or agglutinating, and regulating inflammation. Some of these molecules are also the key components of the acute-phase response.
Role of acute phase proteins during COVID-19
The membrane C-type lectins are cellular sensors that recognize the SARS-CoV-2 spike (S) protein. Similarly, endosomal toll-like receptors (TLRs) recognize their nucleic acids. Some acute-phase proteins, such as MBL, recognize some SARS-CoV-2 S and exhibit antiviral activity by activating the complement lectin pathway, thus contributing to immunological effects during severe illness. Though studies have not uncovered in vivo function of PTX3, unlike C-reactive protein, it binds the viral nucleoprotein.
Despite limited knowledge of how some acute-phase proteins have clinical significance during viral infections, these molecules have served as vital diagnostic tools in outpatient settings to intensive care units (ICUs) throughout the COVID-19 pandemic. High plasma concentrations of CRP or ferritin at hospital admission have indicated poor outcomes among COVID-19 patients.
Similarly, studies have correlated the plasma concentration of d-dimer with acute respiratory distress syndrome (ARDS), a condition associated with higher mortality. Another condition in hospitalized patients with COVID-19, widely used for diagnosis of critical illness, is an increased ferritin: transferrin ratio.
The pathogenesis of post-acute sequelae of COVID-19 (PASC), or long COVID, is complex and multi-faceted. SARS-CoV-2 persists in different organs causing persistent inflammation. In some cases, it might reactivate in response to unrelated viruses, e.g., Epstein–Barr virus. The changes in acute-phase protein levels, including CRP and molecules engaged in iron metabolism, might help define inflammation signature(s) predictive of long COVID.
The liver synthesizes most components of the complement system, a central player of the humoral arm of innate immunity. The concentration of complement molecules also increases in patients with COVID-19, suggesting its role in immunopathologic effects. Though there are approximately 50 soluble complement molecules in the circulation, activating molecules (e.g., C3 and factor B) and negative regulators (e.g., C1 inhibitor) are up-regulated during an acute-phase reaction, further underscoring the relevance of complement-mediated immune responses.
Conclusions
The study highlighted that acute-phase proteins and the acute-phase response are essential components of the humoral arm of innate immunity. They are not just innocent bystanders of acute and chronic inflammation. The recent revelation that select acute-phase proteins are not merely biomarkers but could be used as therapeutic targets is encouraging.
For instance, the serum amyloid P component (SAP) could be a therapeutic target in amyloidosis, even in neurological diseases. It is under clinical evaluation in a randomized phase III trial for idiopathic pulmonary fibrosis treatment. Preclinical studies have suggested that SAP and PTX3 might have therapeutic potential against aspergillus infections. Recent studies have pointed out that MBL could mediate resistance to SARS-CoV-2 infection.
Overall, there is a need to explore selected acute-phase proteins for therapeutic applications.
Timely prediction of a fatal disease, such as COVID-19, is crucial. In this regard, a low-cost molecular signature using CRP and PTX3 as indicators of systemic inflammation and tissue reactions could prove immensely helpful to diagnosticians. Also, these might pave the way to personalized and more patient-centric diagnostics for COVID-19. However, it would require rigorous assessment in large-scale population studies with sustainable technology.