Similar to genes, human microbiota can be passed from mother to child. Early microbiota has exhibited more flexibility than that of adults, and changes in this microbial population affect future development. Recently, scientists reviewed the existing literature to better understand maternal-infant microbiota transmission. This review is available in the journal Neuroscience and Biobehavioral Reviews.
The gut microbial population is extremely complex, which influences human metabolism. In addition, it regulates the expression of around 10% of host transcription genes through metabolism, proliferation, and cellular immunity. Notably, the gut microbiome supplies the host with important amino acids, peptides, vitamins, and antibiotics. Metabolites from the gut microbiome are also associated with the regulation of various functions, including the brain through the gut-brain axis.
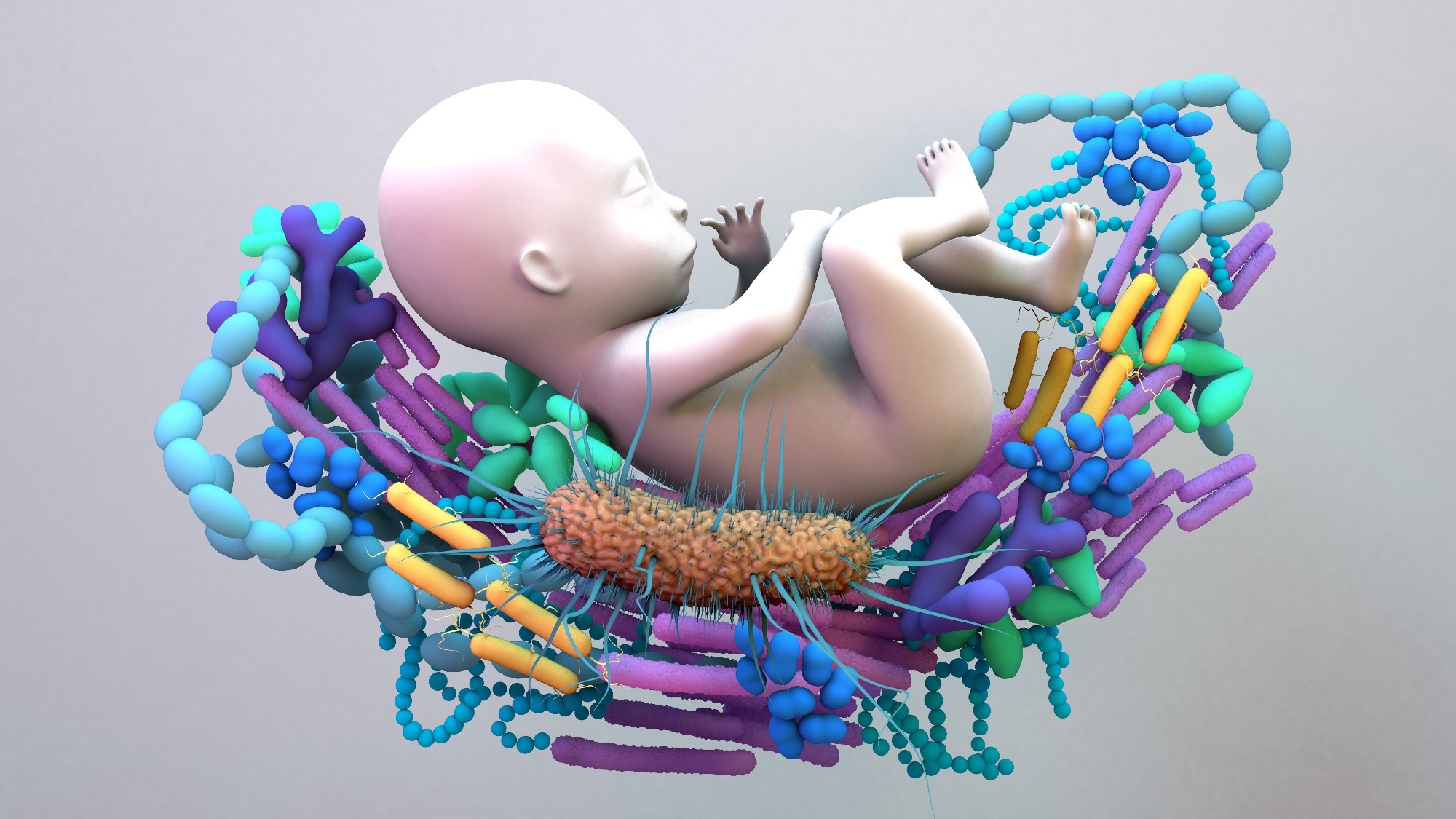 Study: Impact of the mother's gut microbiota on infant microbiome and brain development. Image Credit: Design_Cells / Shutterstock
Study: Impact of the mother's gut microbiota on infant microbiome and brain development. Image Credit: Design_Cells / Shutterstock
Maternal Microbiota During Pregnancy, Birth, and Infancy
Microbiota influences an individual’s health from birth to maturity. The mother and child share a microbiological connection, which is formed in an early phase of life. The newborn's skin and mucosal surfaces are introduced to maternal microbiota, which has a crucial impact on childhood development. These microbes predominantly protect the child from many diseases and are associated with long-term wellness.
The newborn’s microbiota is influenced by genes and the environment. It was previously thought that microbes that ascent out from the vagina were promoters of intrauterine illnesses in the embryo. However, recent research has claimed that microbiota in the gut and mouth are related to fetal health as they are introduced to the bloodstream.
Notably, the maternal microbiome in the stomach, vagina, and oral cavity undergo changes throughout the pregnancy. Some of the factors that are linked to these microbial modifications are medication use, nutrition, stress, and host genomes. In the case of vaginal microbiota (VM), pregnant women have a more stable microbial population than non-pregnant women.
VM is linked to female health, particularly adverse pregnancy outcomes. Women with malnutrition are susceptible to a higher inflammatory reaction to VM, which could lead to unexpected premature labor. Generally, the VM has an abundance of Lactobacillus species. Pregnant women with low Lactobacilli levels are at a higher risk of premature labor.
Previous research claimed the uterus to be sterile; however, recent studies have disagreed with this information. Even though microbes have been detected in the endometrium, not many studies related to endometrial microbiota are available. In addition, there is a dearth of research related to the role of endometrial microbiota in embryonic development and pregnancy fate.
Breastfeeding enhances the Bifidobacterium population in an infant’s guts. The complex interplay between breast milk cytokines and microbiome plays an important role in the regulation of infants’ immunologic, microbial, and metabolic processes.
Although both pregnant and non-pregnant women share a similar microbial composition, there is a difference in abundance and distribution. A reduced gut microbial diversity has an adverse effect on maternal and newborn’s health. Based on a study on rodents, consistent hypertension interferes with gut microbial composition throughout the pregnancy.
Transfer of Microbiota from Mother to Child
The establishment of a microbiome in an infant’s gastrointestinal tract occurs via vertical transfer from the mother to the baby. Microbes are vertically passed from the maternal gut, breast milk, and VM to a child. Microorganisms are found in the mouth, skin, intestine, urogenital tract, and respiratory system of humans.
The most diverse and abundant microbes are found in the intestines. The majority of bacterial species found in a newborn’s stomach are introduced through the maternal vagina, skin, intestine, and mouth. The presence of microbiota in amniotic fluid and placental tissues confirms microbial transfer from mother to child.
Around 100 trillion microbes that, include bacteria, fungi, archaea, and viruses, are found in the human gut. Among all microbes, the bacterial population is significantly higher compared to other microbes. Infants are introduced to diverse microbes from their mother and surrounding environment. Scientists have isolated Streptococci Enterobacteria and Clostridia from infants’ guts during the first two days of their life. On the third day of an infant’s life, 40% of babies have been seen to contain Bacteroides, Clostridia, and Bifidobacteria in their gut.
The Bifidobacteria population increases during the nursing stage of the newborn. Once the baby starts eating solid food, the gut microbiome gets modified and becomes similar to that of adults. During this phase, the prevalence of Firmicutes Enterococcus, Lactobacillus, Staphylococcus, and Clostridium increases substantially.
Several studies have indicated that gut microbiota in the early phase of an infant’s life plays a crucial role in the child’s future health and development. Changes in the vertical transmission of maternal gut microbiome to newborns influence the development of the endocrine, immunological, metabolic, and neurological pathways of the child.
Alteration in vertical transmission of the maternal microbiome to a child is promoted through various factors, such as feeding technique, delivery type, nutrition, mother age at birth, and antibiotic use. For instance, infants who are vaginally delivered have a higher abundance of Lactobacillus in their skin, oral cavities, and gastrointestinal tracts at birth. In contrast, babies delivered via Caesarean section lack Lactobacillus and have higher levels of common skin and environmental microorganisms, such as Propionibacteria, Staphylococcus, and Streptococcus, in their skin, mouth, and gut.