Recently, bacteriocins, synthetic antimicrobial peptides produced by bacteriophages (phages), are being developed as precision antimicrobials. This antimicrobial agent targets specific cell wall hydrolases, such as phage-derived endolysins, for their particular function.
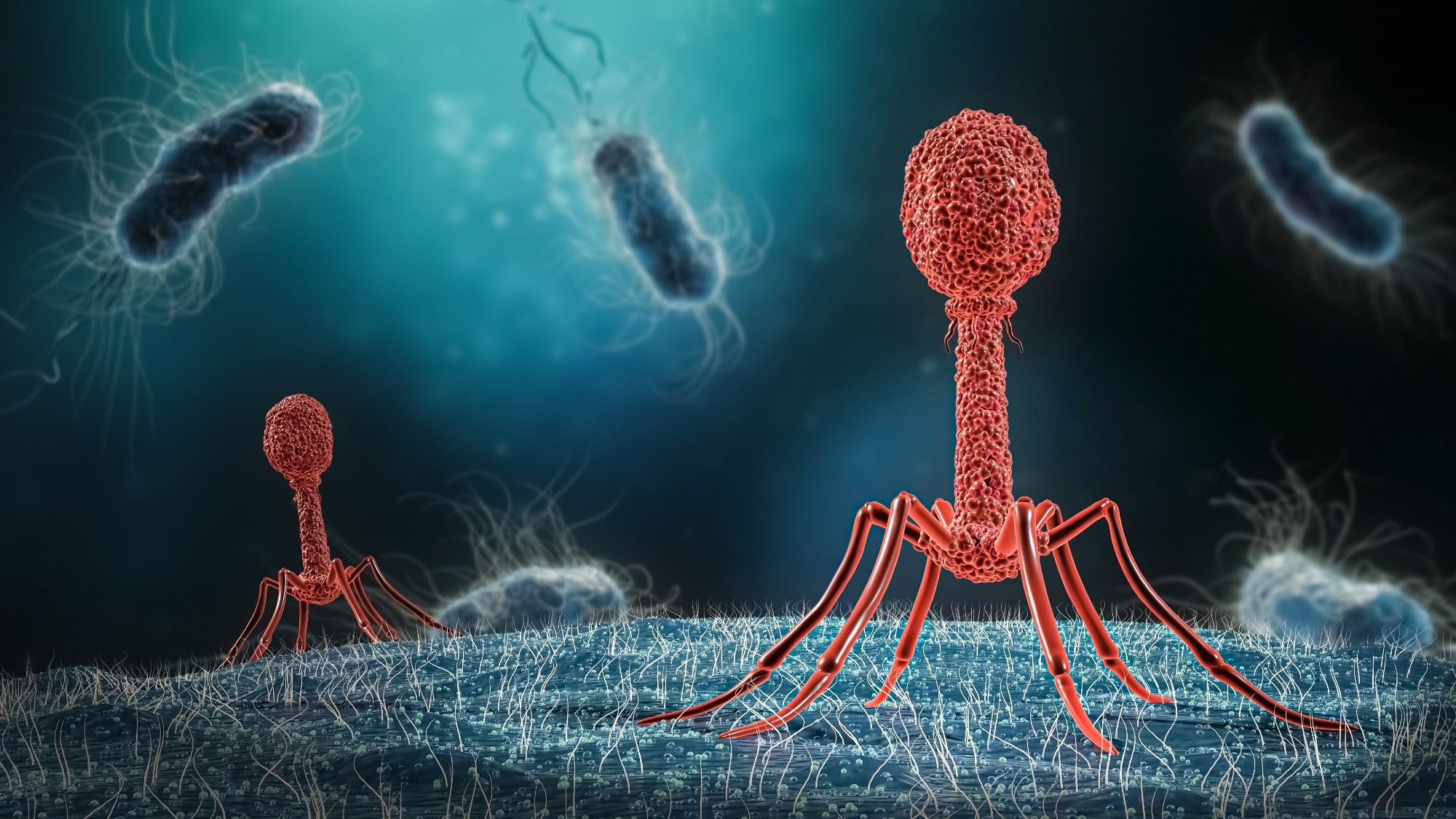 Study: Enhancing bacteriophage therapeutics through in situ production and release of heterologous antimicrobial effectors. Image Credit: MattL_Images/Shutterstock.com
Study: Enhancing bacteriophage therapeutics through in situ production and release of heterologous antimicrobial effectors. Image Credit: MattL_Images/Shutterstock.com
Background
Currently, the most effective bacterial infection treatment is small-molecule antibiotics that target a broad spectrum of pathogenic bacteria.
The global emergence and transmission of antimicrobial resistance (AMR) underscores the need for novel and pathogen-specific antimicrobial treatments. This type of intervention will also prevent antibiotic-induced microbiome dysbiosis.
Phages are important in therapeutics due to their pathogen specificity, ubiquity, and self-replication capacity. Even though the removal of host bacteria by phages is mostly independent of the host drug-resistance profile, this treatment often fails to eliminate all targeted bacterial cells.
This shortcoming of phages could be due to an unknown resistance mechanism or phage tolerance, which could be developed to counteract viral predation.
Previous studies have identified several mechanisms associated with phage resistance or tolerance, including the production of extracellular matrices, adaptive CRISPR-Cas immunity, mutation or reduced expression of phage receptors, restriction/modification systems, and abortive infection systems.
Advancements in synthetic biology and CRISPR-Cas technology have enabled the modification of phage genomes beyond the common model phages, such as T4, T7, or lambda.
Genetic engineering has created sequence-specific antimicrobials via phage-mediated and pathogen-specific delivery of programmed CRISPR-Cas modules.
Through directed receptor binding protein modification, the engineered phase is designed to adapt phage tropism. The engineered phage is also employed to deliver toxic proteins as genetic payloads and is used in diagnostics.
Urinary tract infections (UTIs) are among the most common microbial conditions affecting all age groups. It is a major public health concern, which accounts for more than 2.8 billion US dollars annually.
Although the most common causative agent of UTIs is Escherichia coli, a wide spectrum of Gram-positive, Gram-negative, and fungi also causes UTIs.
About the study
This study used UTIs as a model to demonstrate how HEPTs can function as precision antimicrobials against UTI pathogens. This study revealed that HEPTs suppress resistance and enhance the killing of uropathogenic through dual phage- and effector-mediated targeting.
The current study analyzed 339 isolates obtained from 227 incidents of UTI in Zurich, Switzerland, in 2020. A total of 25 different bacterial species were identified. Among these, the top three abundant uropathogens were E. coli, Enterococcus faecalis, and Klebsiella pneumoniae.
Study findings
In this study, HEPTs were constructed using five distinct lytic phages that target uropathogens, namely, E. coli (phages E2 and CM001), E. faecalis (phages EfS3 and EfS7) and K. pneumoniae (phage K1).
For Gram-negative uropathogens, four colicin-like bacteriocins (CLBs) were selected as effectors. These were active against E. coli and K. pneumoniae. For E. faecalis, which is a Gram-positive uropathogen, a phage-derived chimeric cell wall-hydrolase (EC300) was employed that recognized and disrupted the bacterial cell walls with high specificity.
All effector genes were genetically optimized to target specific pathogens, and these were incorporated within the phage genome.
A total of 14 HEPTs were constructed based on five distinct phage scaffolds that comprised five different payload genes. These HEPT candidates were developed using CRISPR-Cas9-assisted engineering or rebooting synthetic genomes in suitable surrogate hosts.
In order to avoid toxicity and fitness costs, CLB-encoding HEPTs were constructed and amplified based on respective bacteriocin immunity proteins.
All developed effector proteins were active against a wide spectrum of urine-derived isolates, particularly the target species, with variable levels of efficacy. The experimental findings indicated that the developed HEPTs acted as effective precision antimicrobials.
This role was demonstrated based on their pathogen-specific killing activity of bacteriophages with in situ production and release of secondary antimicrobial effectors. This mechanism enabled the suppression of phage-resistant subpopulations.
Furthermore, a single HEPT or HEPT cocktail could be used to cross-genus control bacterial pathogens. Compared to the wild-type phage, a colicin E7-producing HEPT exhibited superior control of patient E. coli bacteriuria.
Conclusions
The current study focussed on developing HEPTs as a precision antimicrobial agent against UTI pathogens. Notably, HEPTs offered many advantages in accordance with developmental, therapeutic, and translational perspectives.
Here, the newly developed HEPTs could suppress resistance and enhance uropathogen killing via dual phage- and effector-mediated targeting. The HEPTs were designed to control polymicrobial uropathogen communities by producing effectors with cross-genus activity.
This study highlighted the importance of phages with heterologous effectors for effective UTI treatment. This approach could be a versatile tool to enhance and adapt phage-based precision antimicrobials.