CAC is a measure of atherosclerosis and predicts coronary artery disease (CAD) events. Coronary calcification is a manifestation of atherosclerotic plaque. It is suggested to contribute to plaque rupture when present as microcalcifications, while more extensive calcification sheets are associated with stabilizing the plaque.
Vascular calcification is characterized by the contractile-to-osteogenic phenotype switch of vascular smooth muscle cells (VSMCs). The osteogenic phenotype is characterized by the expression of markers, including the master regulator of the switch, Runt-related transcription factor 2 (RUNX2), and others such as alkaline phosphatase (ALPL) and bone gamma-carboxyglutamate protein (BGLAP).
Genome-wide association studies (GWASs) have identified more than 200 loci associated with CAD events and only four for CAC. The four CAC loci are also associated with CAD events, and their effects are mainly related to the progression of atherosclerosis. Identifying additional loci for CAC will provide insights into the pathogenic mechanism of atherosclerotic cardiovascular disease.
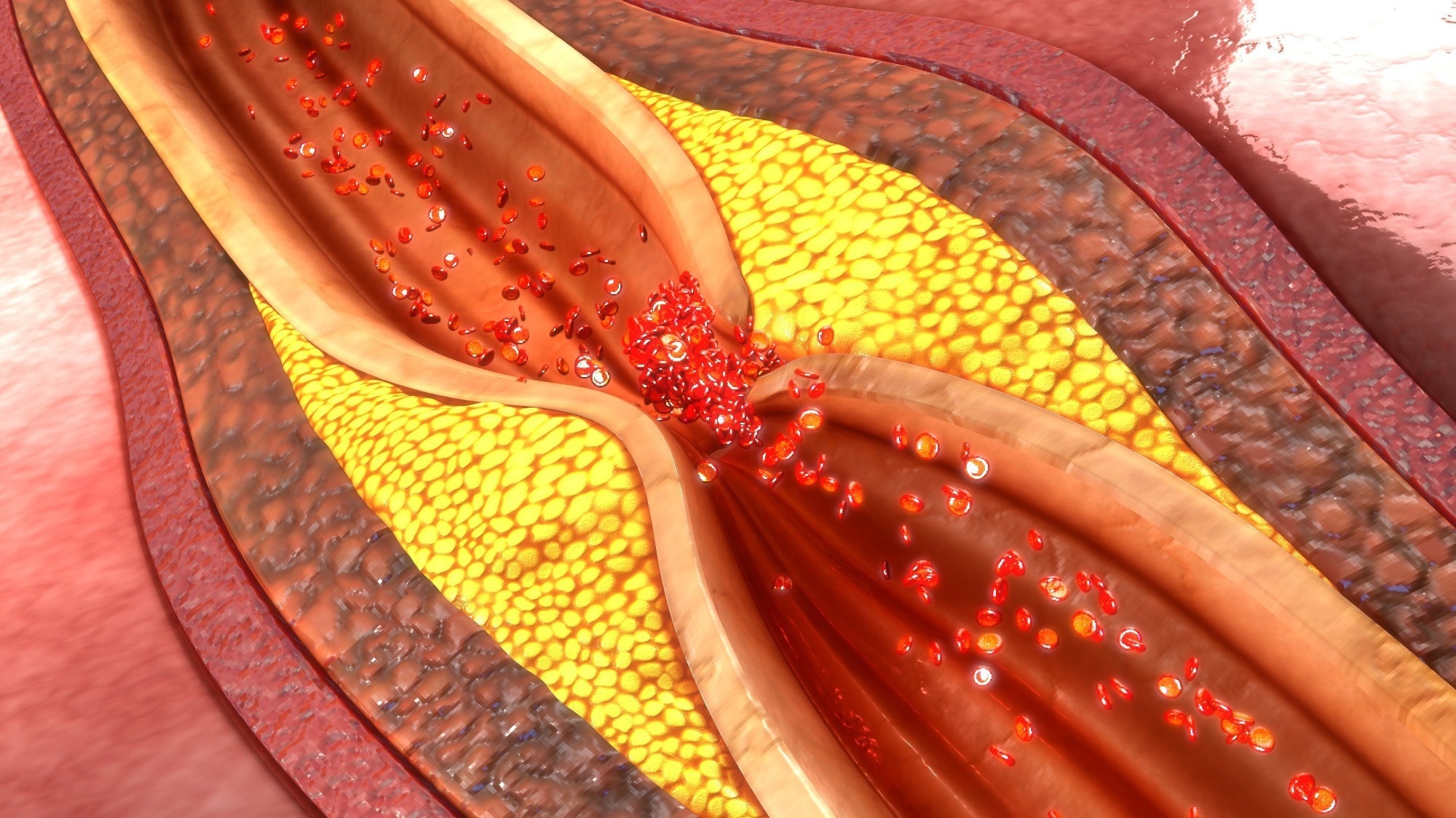 Letter: Whole-genome sequencing uncovers two loci for coronary artery calcification and identifies ARSE as a regulator of vascular calcification. Image Credit: sciencepics / Shutterstock
Letter: Whole-genome sequencing uncovers two loci for coronary artery calcification and identifies ARSE as a regulator of vascular calcification. Image Credit: sciencepics / Shutterstock
The study and findings
In the present study, researchers performed a GWAS to identify CAC loci. Around 22,400 individuals from 10 studies, with whole-genome sequencing and CAC data, were included and stratified based on race/ethnicity. Participants were an average age of 58, 53% male and 47% female. Half the population had detectable CAC. In single-variant analyses, over 28.5 million variants with minor allele count ≥ 50 were tested for associations with CAC.
Genetic variants showing a significant association with CAC were detected at six loci – 9p21, matrix metallopeptidase 16 (MMP16), apolipoprotein B (APOB), APOE, arylsulfatase E (ARSE), and phosphatase and actin regulator 1/endothelin 1 (PHACTR1/EDN1). Next, rare variants (minor allele frequency < 1%) were tested for associations with CAC using gene-based variant aggregation and filtering. This resulted in a genome-wide significant aggregation unit for CAC mapping to APOB.
However, the associations were insignificant when adjusted for the index variant identified at that locus in the single-variant analysis. Genetic variants in MMP16 and ARSE were not previously reported to be associated with CAD or CAC at a genome-wide significance level. The inverse association between CAC and the G allele of the ARSE index variant (rs5982944) followed a recessive mode of inheritance.
Further, the index variant at ARSE was associated with carotid plaque, low- (LDL-C) and high-density lipoprotein cholesterol (HDL-C), and systolic blood pressure. It was also associated with thoracic ascending and descending aorta calcification. On the other hand, the MMP16 index variant (rs13268080) showed nominal associations with CAD events and was not significantly associated with any other atherosclerotic phenotypes.
Moreover, the credible set analysis suggested that the ARSE index variant was the causal variant with an 85% posterior probability. This variant was also associated with ARSE gene expression levels in various cells and tissues, such as the aorta and cultured fibroblasts. The G allele of the ARSE index variant was associated with lower ARSE expression in cultured fibroblasts, suggesting that increased ARSE levels might stimulate arterial calcification.
Likewise, the MMP16 index variant was associated with MMP16 gene expression. The G allele of this variant in the aorta was associated with reduced MMP16 messenger RNA (mRNA) levels. Further analyses suggested that increased MMP16 expression might inhibit calcification. Next, functional perturbation analyses were performed in coronary artery VSMCs to examine whether ARSE and MMP16 regulate the phenotypic switch and calcification.
MMP16 expression in VSMCs was reduced by 75% when grown in osteogenic media relative to normal media. Silencing MMP16 had no effect on the osteogenic phenotype or calcification of VSMCs. By contrast, ARSE expression increased five-fold (mRNA) and 1.7-fold (protein) when VSMCs were grown in osteogenic media compared to normal media.
Silencing ARSE decreased the expression of osteogenic phenotype markers (RUNX2, ALPL, and BGLAP) and increased that of calponin (contractile phenotype marker). It also reduced calcium deposition by cells in osteogenic media by 60% and increased cellular contractility. Increasing ARSE levels in VSMCs in normal media caused a seven-fold increase in RUNX2 and a 70% reduction in calponin levels.
Further, coronary VSMC calcification increased four-fold, and coronary artery contractility declined by 70%. When experiments were performed using aortic VSMCs, results were similar to those in coronary artery VSMCs. Next, ARSE expression was examined in the coronary arteries of ischemic CAD patients and controls.
ARSE expression was low in coronary arteries from controls but significantly higher in patients. RUNX2 expression was also higher in calcified ischemic arteries, and it co-localized with ARSE. Additional experiments revealed that the ARSE index variant could influence ARSE gene expression in HEK293 cells and human aortic and coronary artery smooth muscle cells.
Conclusions
Together, six loci associated with CAC were identified. The ARSE index variant was restricted to populations with African ancestry. The findings implicate ARSE as a regulator of the phenotype switch and calcification. ARSE silencing increased VSMC contractility but decreased osteogenic phenotype markers and calcification, while its overexpression induced opposite effects. Overall, the results underscore ARSE as a potential drug target for vascular calcific disease.