In a recent study published in the journal Cell, researchers investigated the infectivity, fusogenicity, and immune evasive potential of two novel Omicron subvariants – BA.2.86 and FLip. They used sera from healthcare workers under varying monovalent, bivalent, and multi-dose vaccination regimes. Their tests on human cell lines infected with these new strains reveal that, while not as immune evasive as older Omicron variants, BA.2.86 presents significant mutations in its spike proteins, potentially altering its biology and imparting high infectivity to the subvariant. Alarmingly, most conventional antibodies proved unable to neutralize BA.2.86, highlighting the need for constant subvariant monitoring and vaccine updating to prevent a resurgence of the COVID-19 pandemic.
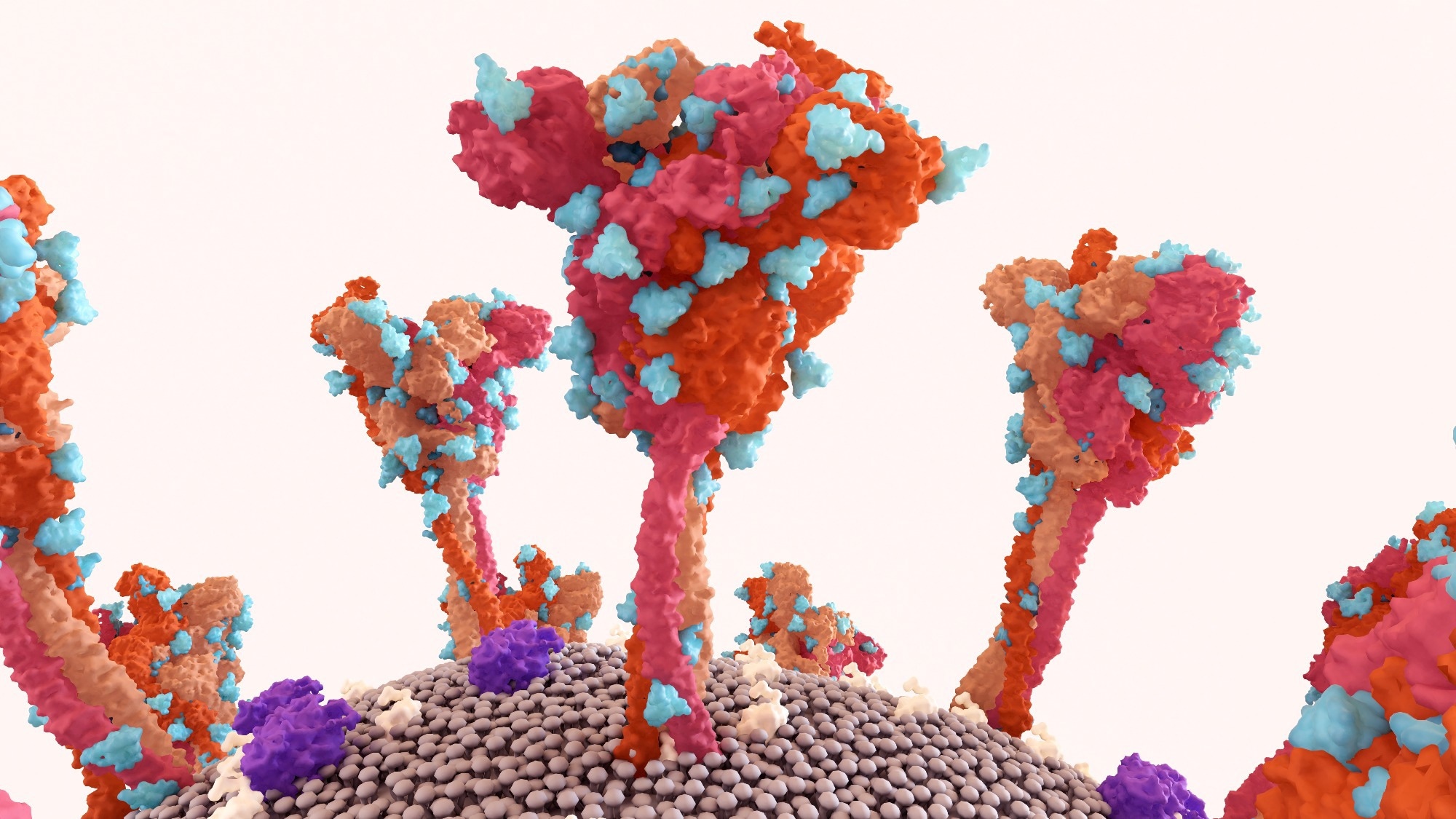 Study: Immune evasion, infectivity, and fusogenicity of SARS-CoV-2 BA.2.86 and FLip variants. Image Credit: Design_Cells / Shutterstock
Study: Immune evasion, infectivity, and fusogenicity of SARS-CoV-2 BA.2.86 and FLip variants. Image Credit: Design_Cells / Shutterstock
COVID-19 and the dangers of its subvariants
The coronavirus disease 2019 (COVID-19) pandemic has infected more than 700 million individuals and claimed almost 7 million lives since the onset of the pandemic in late 2019. Caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus, COVID-19 represents one of the worst pandemics in human history, resulting in devastating global losses to infrastructure, economy, and quality of life. Furthermore, more than 60% of survivors experience persistent COVID-like symptoms months or even years following initial infection recovery, further exacerbating the disease’s burden.
SARS-CoV-2 is a positive-sense single-stranded RNA virus belonging to the genus Sarbecovirus. The bulk of the pathogen’s infectivity can be attributed to its spike proteins, the surface proteins containing the receptor binding domains (RBDs) that allow the virus to attach to and invade host cells. Vaccines, especially those comprising monoclonal antibodies (mAbs), are designed to target and inactivate these RBDs, thereby neutralizing SARS-CoV-2’s ability to invade and hijack its host cells.
Unfortunately, like all members of its genus, SARS-CoV-2 presents an exceptionally high mutation rate, resulting in thousands of variants and subvariants, only a fraction of which have been discovered and characterized thus far. While most variants retain their ancestor’s spike protein genetic sequence and can, therefore, be neutralized by vaccines targeting their ancestral strain, mutations in some strains’ RBDs can significantly alter their biology and clinical pathology and, worse, render conventional vaccines ineffective.
Omicron (ancestral BA.2) is the most recent, prevalent, and hitherto most infectious clade of SARS-CoV-2 variants. Its sub-lineage XBB 1.5 is the most transmissible of any characterized variant and forms the bulk of today’s COVID-19 burden. Despite global vaccination efforts and government-enforced social-distancing measures curbing the spread of the disease, the emergence of new variants of concern (VOCs) has driven extensive research aimed at characterizing novel strains and the efficacy of conventional vaccines against them.
BA.2.86 and FLip are two relatively novel Omicron subvariants initially discovered in late July 2023. BA.2.86 is medically especially concerning given that its spike protein presents more than 30 mutations relative to its ancestral BA.2 (Omicron) and 35 mutations relative to XBB 1.5, the target of the currently available vaccine. This evolutionary jump is alarming due to it being comparable to the divergence of Omicron from the original Wuhan-Hu-1 SARS-CoV-2 strain.
“Given that BA.2.86 spike is notably distinct from XBB.1.5, there is concern that current mRNA vaccines, as well as the updated XBB.1.5 mRNA booster, will not effectively protect against BA.2.86.”
Nicknamed “Pirola,” BA.2.86 has been identified in more than 23 countries with at least 300 confirmed infected. Investigating the pathology of this and other VOCs will provide medical practitioners with the information they require to prepare for localized outbreaks. Conventional vaccine efficacy investigations will, in turn, allow vaccine manufacturers important insights when designing the next generation of anti-COVID vaccines.
About the study
In the present study, researchers investigated the infectivity of BA.2.86 and FLip relative to D614G, Omicron BA.1, BA.2, BA.4/5, and EG.5.1 in two cell lines - human embryonic kidney cell line (HEK293T), and human lung adenocarcinoma cell line (CaLu-3). They further used serum samples collected from healthcare workers vaccinated with either three doses of monovalent mRNA vaccines (N = 15), or a combination of two doses of monovalent mRNA vaccine supplemented with one dose of bivalent vaccine (N = 14) to investigate the efficacy of conventional Moderna mRNA-1273 and Pfizer BioNTech BNT162b2 vaccines against these emergent subvariants.
Additionally, the monoclonal antibody S309, notable as being effective against a broad spectrum of Omicron variants, including EG.5.1 and XBB 1.5, was added to the investigation to verify if it could comprise the next generation of protection against BA.2.86 and FLip. Fusogenicity was estimated using cell lines cotransfected with subvariant spike proteins and enhanced green fluorescent protein (eGFP). Luminescence readouts were used to evaluate the degree of cell-cell fusion between spike proteins and ACE2 receptors (the receptors to which SARS-CoV-2 RBDs bind).
Finally, the spike protein of BA.2.86 was structurally modeled to elucidate its affinity to the ACE2 receptor and to estimate the degree of neutralization by conventional vaccines. Neutralizing antibody titers were computed using antigenic mapping assays.
Study findings
Antigenic distance evaluations revealed that BA.2.86 has significantly lower immune evaluation capabilities compared to previous XBB subvariants and FLip. Alarmingly, however, S309 antibodies, effective against XBB variants, were ineffective at neutralizing BA.2.86. Structural modeling depicts that this may be due to mutations in the D339H region, altering the spike protein and, in turn, drastically reducing the antibody efficacy.
Infectivity analyses revealed that BA.2.86 was not as infectious as other XBB subvariants in ACE-2-expressing HEK293T cells but was significantly higher in CaLu-3 cells. These findings were mirrored in fusogenicity evaluations, together suggesting conformational changes in the virus and highlighting a potential alteration in its biology and pathology.
Encouragingly, sera from healthcare workers immunized with Moderna mRNA vaccines designed against XBB 1.5 were effective in neutralizing both FLip and BA.2.86. However, the affinity and enhanced infectivity of BA.2.86 for CaLu-3 may suggest an altered mode of infection (plasma membrane fusion pathway in place of the endosomal pathways used by most XBB subvariants), thereby potentially necessitating vaccination updates.
“Whether or not BA.2.86 will have an increased lung tropism, and thus enhanced pathogenesis compared to other Omicron variants, is unknown and needs to be carefully examined.”
Journal reference:
- Qu, P., Xu, K., Faraone, J. N., Goodarzi, N., Zheng, Y.-M., Carlin, C., Bednash, J. S., Horowitz, J. C., Mallampalli, R. K., Saif, L. J., Oltz, E. M., Jones, D., Gumina, R. J., & Liu, S.-L. (2024). Immune evasion, infectivity, and fusogenicity of SARS-CoV-2 BA.2.86 and FLip variants. In Cell, DOI – https://doi.org/10.1016/j.cell.2023.12.026, Publication link – https://www.cell.com/cell/fulltext/S0092-8674(23)01400-9