A growing area of research is the association between dietary patterns and cognitive health, especially related to understanding the modifiable risk factors for dementia and other neurodegenerative diseases. Findings from various reviews and meta-analyses have found that diets rich in fruits, whole grains, and vegetables are beneficial for cognitive health.
However, findings from individual studies about dietary patterns such as the Dietary Approach to Stop Hypertension (DASH), Mediterranean, anti-inflammatory, and Mediterranean-DASH diet Intervention for Neurodegenerative Delay (MIND) diets have been inconsistent. These inconsistencies, stemming from heterogeneity in the methods for conducting dietary and cognitive assessments, study populations, follow-up durations, and various other study parameters, have made it challenging to conclude potential dietary guidelines for cognitive health.
A proposed approach to draw inferences from these heterogeneous individual studies involves pooling individual participant data from various clinical and observational trials, similar to a meta-analysis. It differs from a meta-analysis in that the data is sought from the eligible study rather than extracted from the publication. However, a method of harmonizing the data is still required to ensure comparability and compatibility across the data.
About the study
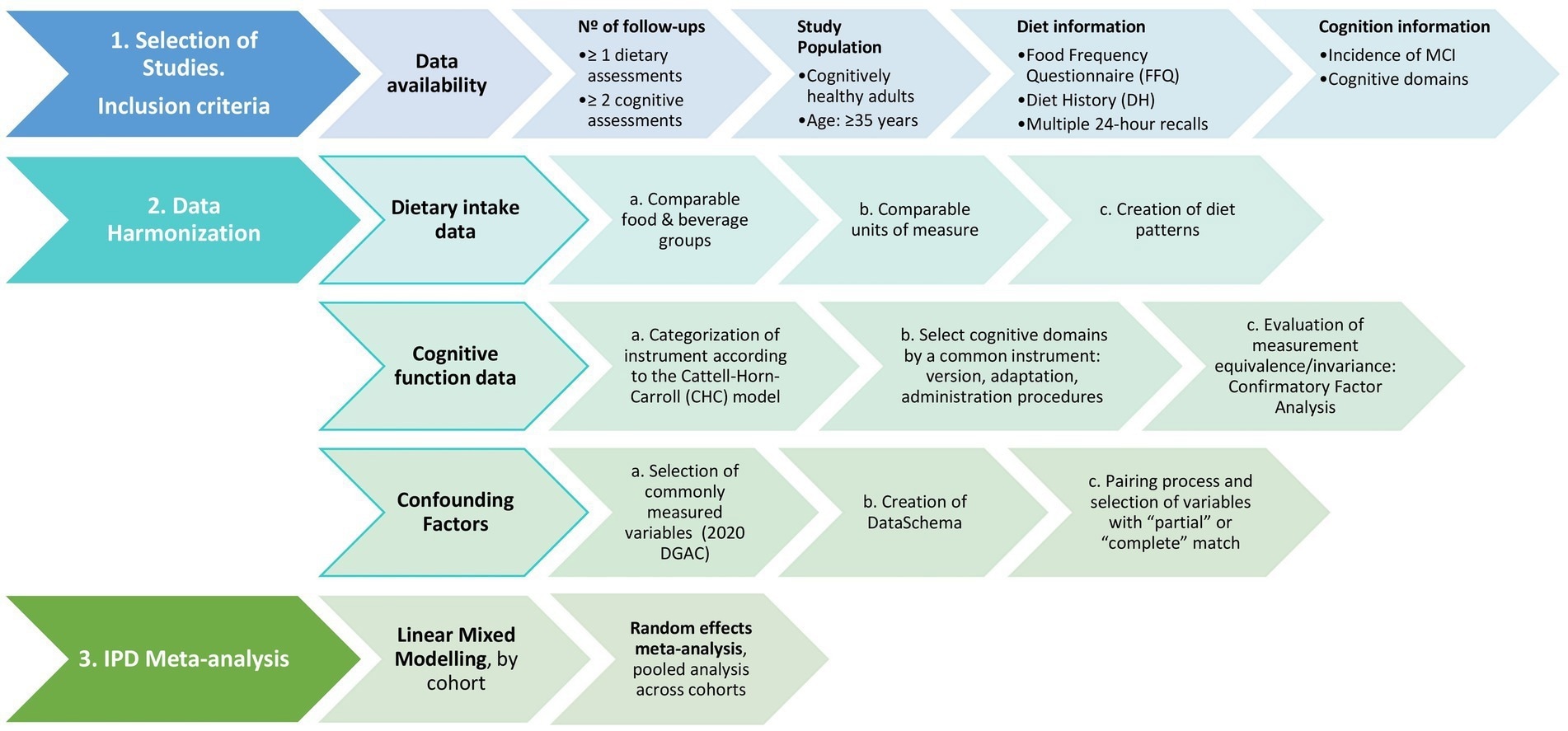
The present study described a protocol for retrospectively harmonizing individual participant data from numerous studies from the United States (U.S.) and Europe on the association between dietary patterns and cognitive health. They also discussed the study selection criteria to address the study question and provided definitions for the outcomes and exposures of the study.
Harmonization of data
To determine the associations between dietary patterns and the incidence of cognitive decline and mild cognitive impairment, the selection criteria stipulated the inclusion of studies that examined diets representative of different populations across the U.S. and Europe, with the study design being either a clinical trial or a prospective cohort study. Only studies conducted on adults above the age of 35 who were cognitively healthy were to be included in the harmonization analysis. Sensitivity analyses were recommended to assess the interactive effects of comorbidities such as obesity, cardiovascular disease, diabetes, depression, and physical activity.
The exposures considered for the analysis comprise dietary patterns such as adaptations of the Mediterranean diet pattern, EAT-Lancet pattern, the Healthy Eating Index, or a pattern derived a posteriori from the results of a principal component analysis. Diet history, food frequency questionnaires, or data from repeat interviews would be used to determine the daily food intake scores.
The outcomes for the analysis consist of cognitive performance assessments at two time points to determine changes in cognition or the development of mild cognitive impairment. The data on dietary patterns would be harmonized into groups of foods and beverages such as dairy, vegetables, fruits, meat, candy, and sugar-sweetened beverages.
The researchers also recommended ensuring that the units used report the nutrients were converted to one unit and reported along with the number of grams in one serving of each food category. The harmonized dietary data would consist of one exposure variable for healthy dietary patterns, reported in terms of a score such as the Healthy Eating Index.
The proposed method for harmonizing individual participant data suggested that only those instruments of cognitive measures that can potentially diagnose mild cognitive impairment or measure executive function, verbal fluency, and verbal memory be included in the analysis. Additionally, the cognitive data should be harmonized using pre-statistical harmonization to categorize the cognitive tests from each study according to the cognitive abilities being examined.
 Schematic study protocol to assess the association between diet patterns and cognitive decline.
Schematic study protocol to assess the association between diet patterns and cognitive decline.
Data augmentation strategies were suggested to address possible heterogeneity across factors such as administration of cognitive measurements, instrument adaptation, components, and instrument version. Furthermore, a confirmatory factor analysis will be used to test the equivalence of the cognitive measurements.
The study also discussed methods to harmonize data on confounding factors such as lifestyles, physical activity, sociodemographic factors, anthropometry, and physical activity levels. The harmonized data on dietary intake, cognitive measures, and confounding factors will then be used to determine the association between diet and cognitive health through an individual participant data meta-analysis.
Conclusions
To summarize, the study provides a method to harmonize data from numerous heterogeneous studies so that the study design can infer the association between dietary patterns and cognitive health. The application of this method and the findings will help formulate dietary guidance recommendations to improve cognitive health and prevent cognitive decline.