The World Health Assembly established the EPI in 1974, marking a significant commitment to extend the benefits of vaccination to all. The WHO launched the initiative to initially vaccinate children against measles, poliomyelitis, smallpox, pertussis, tetanus, diphtheria, and tuberculosis by 1990. Currently, the EPI includes protection against other pathogens across all ages. This growth in vaccination programs covering more diseases has led to a massive increase in the breadth of protection.
 Study: Contribution of vaccination to improved survival and health: modelling 50 years of the Expanded Programme on Immunization. Image Credit: Riccardo Mayer / Shutterstock
Study: Contribution of vaccination to improved survival and health: modelling 50 years of the Expanded Programme on Immunization. Image Credit: Riccardo Mayer / Shutterstock
About the study
In the present study, researchers modeled the impact of EPI on public health. They estimated the number of deaths prevented, years of full health gained (i.e., disability-adjusted life-years averted), and years of life gained by vaccination against 14 pathogens between June 1974 and May 2024 in WHO member states.
Vaccinations for the following pathogens/diseases were introduced: tuberculosis, yellow fever, Haemophilus influenzae type B, diphtheria, Japanese encephalitis, pertussis, measles, rotavirus, poliomyelitis, rubella, invasive pneumococcal disease, tetanus, meningitis A, and hepatitis B. A standardized framework was developed to assess the impact per fully vaccinated individual.
The team synthesized vaccine coverage estimates from WHO’s Polio Information System, Supplementary Immunization Activities Database, Immunization dashboard, and Vaccine Impact Modeling Consortium (VIMC). Overall, 24 vaccine activities were evaluated, stratified by disease, vaccine, dose number, and routine or supplementary immunization. Modeling was performed in three forms.
First, impact estimates were derived by simulating published transmission models for poliomyelitis and measles for the 50-year period. Second, VIMC transmission models were extended for hepatitis B, rotavirus, rubella, H. influenzae type B, invasive pneumococcal disease, and Japanese encephalitis from 2000 to 2024. Third, static disease burden models for tuberculosis, pertussis, tetanus, and diphtheria were upgraded.
The three forms of modeling allowed for capturing individual- and population-level vaccine effects. The primary outcome was estimating the impact of EPI on deaths averted, years of life gained, years of full health gained, and the proportion of vaccination-attributable reduction in infant mortality. Additionally, as secondary outcomes, these measures were evaluated by the World Bank income strata and region.
Findings
The researchers estimated that vaccination programs for the 14 pathogens had averted around 154 million deaths between June 1974 and May 2024; this included 146 million deaths averted in those younger than five. Further, 10.2 billion years of full health and nine billion life-years were gained in this period. On average, 66 years of full health and 58 years of life were gained.
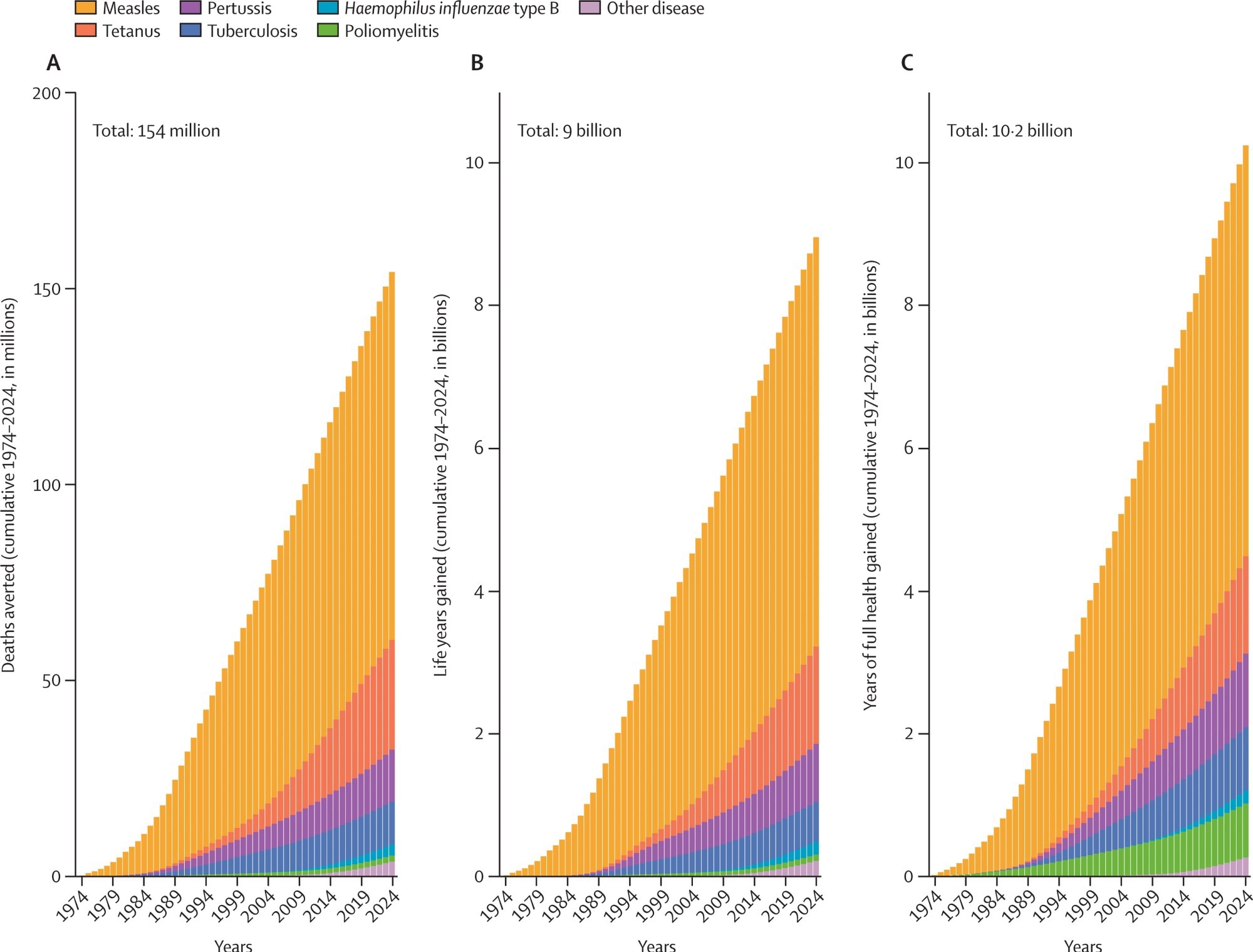
Deaths averted, years of life saved, and years of full health gained due to vaccination. Data are cumulative 1974–2024. Measles: deaths averted: 93·7 million; years of life saved: 5·7 billion; years of full health gained: 5·8 billion. Tetanus: deaths averted: 27·9 million; years of life saved: 1·4 billion; years of full health gained: 1·4 billion. Pertussis: deaths averted: 13·2 million; years of life saved: 0·8 billion; years of full health gained: 1 billion. Tuberculosis: deaths averted: 10·9 million; years of life saved: 0·6 billion; years of full health gained: 0·9 billion. Haemophilus influenzae type B: deaths averted: 2·8 million; years of life saved: 0·2 billion; years of full health gained: 0·2 billion. Poliomyelitis: deaths averted: 1·6 million; years of life saved: 0·1 billion; years of full health gained: 0·8 billion. Other diseases: deaths averted: 3·8 million; years of life saved: 0·2 billion; years of full health gained: 0·3 billion.
Notably, 0.8 billion years of full health gained were attributable to averted poliomyelitis cases. Measles vaccination saved 93.7 million lives in 50 years and was the single most significant driver of lives saved across all years in WHO regions and World Bank income strata. Further, there has been a substantial reduction in global infant mortality since 1974, with vaccination directly accounting for 40% of this achievement.
Individuals aged 10, 25, or 50 in 2024 were estimated to be 44%, 35%, or 16% more likely to survive the following year, respectively, compared to a hypothetical scenario of no vaccinations since 1974. The African and Eastern Mediterranean regions showed the most significant absolute gains in life course survival probability, while the European region had the lowest. On the other hand, the European and Western Pacific regions had the largest relative gains, while the African region had the lowest.
Conclusions
The findings show that vaccines have saved an estimated 154 million lives since 1974, a majority (95%) of which were in children under five years. This meant nine billion life-years saved and 10.2 billion years of healthy life gained due to vaccination. Notably, measles vaccination was the single most significant contributor.
Further, vaccination was responsible for nearly half of the global infant mortality reduction. Consequently, a child born in 2024 will have a 40% increased survival yearly. Moreover, the survival benefits of infant vaccination extend beyond 50 years. Regions with initially high mortality had more considerable absolute gains but lower relative gains.