In a recent study published in the International Journal of Impotence Research, a group of researchers assessed the relationship between Coronavirus Disease-19 (COVID-19) and ischemic priapism in patients treated at three university hospitals in Egypt between April 2020 and June 2022. Ischemic priapism is a rare condition where blood gets trapped in the erection chambers of the penis.
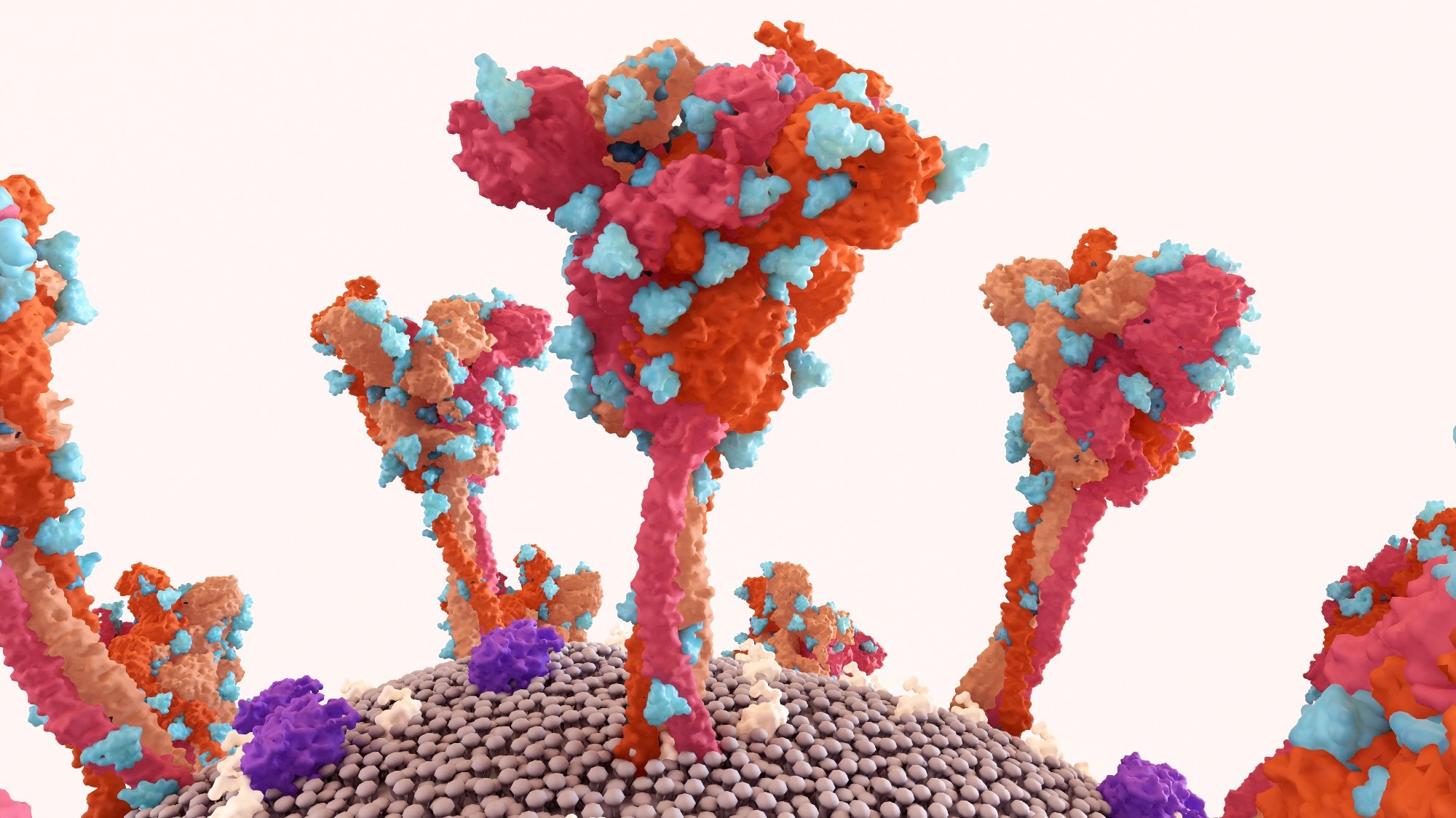 Study: The relationship between Coronavirus Disease-19 (COVID-19) and ischemic priapism: a case-control study. Image Credit: Design_Cells / Shutterstock
Study: The relationship between Coronavirus Disease-19 (COVID-19) and ischemic priapism: a case-control study. Image Credit: Design_Cells / Shutterstock
Background
On March 11, 2020, the World Health Organization (WHO) declared COVID-19 a pandemic. The disease has profoundly impacted medical, social, economic, and environmental aspects of life, leading to widespread lockdowns. By March 24, 2024, the WHO reported 775,132,086 confirmed cases and 7,042,222 deaths. COVID-19 symptoms vary widely, with fever, cough, and anosmia being common. Severe cases often exhibit hypercoagulability, increasing the risk of thromboembolic complications, including ischemic priapism, a urological emergency caused by sinusoidal thrombosis. Further research is needed to determine whether the association between COVID-19 and ischemic priapism is causal or merely coincidental.
About the study
The present study retrospectively reviewed patients with priapism at three university hospitals from April 2020 to June 2022. During the COVID-19 pandemic, all emergency department patients were assessed for COVID-19 using chest computed tomography (CT), complete blood count (CBC), C-reactive protein (CRP), and D-dimer tests, followed by polymerase chain reaction (PCR) for suspicious cases. A positive PCR test confirmed COVID-19 positivity.
Priapism patients were evaluated for duration, pain, drug history, trauma, systemic disease, and recurrence. After informed consent, cavernosal aspiration was performed by inserting a needle into the penile cavernosal tissue, aspirating blood, and irrigating with saline and Ephedrine hydrochloride until detumescence. Blood samples were analyzed, and a distal shunt procedure was performed if detumescence was not achieved within an hour.
Data collected included age, co-morbidity, priapism type, episode duration, cavernous blood gases, chest CT findings, lymphocyte percentage, CRP, D-dimer levels, COVID-19 course, priapism management, and follow-up erectile function. Patients were classified into two groups based on COVID-19 presence, and criteria were compared, including erectile function assessed using the International Index of Erectile Function-5 (IIEF-5). Statistical analysis used the Kolmogrov-Smirnov Z, t-tests, Mann-Whitney U, and Chi-square tests, with significance at p ≤ 0.05.
Study results
During the study period, 43 patients with ischemic priapism were diagnosed, with a median age of 36 years and a median priapism duration of 8 hours. Among these patients, 2.3% had chronic kidney disease, 6.97% had hypertension, and 16.3% had diabetes. The patients were divided into two groups: 30 patients with ischemic priapism only (Group I) and 13 patients with both ischemic priapism and COVID-19 (Group II).
Cavernosal aspiration was successful in 83.3% of patients in Group I and 92.3% in Group II, showing no significant difference (P = 0.4). Recurrence of priapism occurred in 16.7% of patients in Group I, while no recurrences were observed in Group II (P = 0.1). At the last follow-up, moderate erectile dysfunction (ED) developed in 6.7% and severe ED in 13.3% of patients in Group I. In Group I, those with severe ED were managed with a distal shunt and prepared for penile prosthesis placement, except for one patient who developed moderate ED after the distal shunt. In Group II, one patient (7.7%) developed severe ED after distal shunting and was also prepared for penile prosthesis implantation. The median duration of ischemic priapism was significantly longer in patients with severe ED compared to those without (19 vs. 7 hours, P = 0.01).
There were no statistically significant differences between the two groups in terms of age (P = 0.8), required priapism management (P = 0.4), priapism recurrence (P = 0.1), and ED severity (P = 0.5).
In Group II, priapism was the main presenting symptom in 30.8% of patients, leading to the incidental diagnosis of COVID-19. Other patients presented with varying degrees of COVID-19 symptoms: mild in 5 patients, moderate in 2 patients, and severe in 2 patients. Patients with priapism and mild COVID-19 symptoms were treated with home isolation and supportive care, including vitamin C, zinc, lactoferrin, acetylcysteine, paracetamol, and ivermectin. Those with moderate symptoms received similar treatment along with intravenous ivermectin, anticoagulants, and steroids, while severe cases were referred for hospital isolation. All COVID-19 patients recovered completely after treatment.
Patients with mild and moderate COVID-19 symptoms responded well to cavernosal aspiration, maintained erectile function, and did not experience priapism recurrence. Those with severe COVID-19 symptoms also responded well to cavernosal aspiration, with one patient developing mild ED.
Conclusions
To summarize, this study, the largest on ischemic priapism in COVID-19 patients, found that priapism occurred across all COVID-19 severity levels. COVID-19 did not alter priapism treatment protocols or post-treatment erectile function. The findings suggest a coincidental rather than causal relationship between COVID-19 and ischemic priapism.
Journal reference:
- Almekaty, K., Taha, A.E., Ragab, M. et al. The relationship between Coronavirus Disease-19 (COVID-19) and ischemic priapism: a case-control study. Int J Impot Res (2024), DOI - 10.1038/s41443-024-00929-z, https://www.nature.com/articles/s41443-024-00929-z