The U.S. Centers for Disease Control and Prevention (CDC), in association with the University of Iowa, USA, has conducted an epidemiological study to determine the incidence rate of Lyme disease among older adults in the United States.
Lyme disease, also known as Lyme borreliosis, is a vector-borne bacterial infection caused by a species of Borrelia bacteria that spreads to humans by the bite of infected black-legged ticks (Ixodes scapularis). The main symptoms are fever, headache, fatigue, and a specific type of skin rash called erythema migrans.
While Lyme disease can present with a characteristic erythema migrans rash, it can also lead to severe complications if left untreated, including facial nerve paralysis, arthritis, and even heart rhythm irregularities.
In the United States, Lyme disease most commonly occurs in the Northeast, mid-Atlantic, and upper-Midwest regions. Previous studies estimating the prevalence of the disease have used employer-sponsored insurance claims data to quantify the disease diagnoses.
However, this type of data does not include information on individuals aged 65 years and above who exhibit higher susceptibility to Lyme disease than their younger peers.
In this study, scientists have determined the incidence of Lyme disease among older adults in the United States using Medicare fee-for-service data that includes information on individuals aged 65 years and above.
Study design
The study analyzed Medicare fee-for-service data together with drug treatment data to identify Lyme disease diagnoses among individuals aged 65 years and above. The data collected during 2016 – 2019 was included in the analysis.
The Medicare fee-for-service study population was compared with the 2019 US Census estimation data for individuals aged 65 years and above to ensure that the two groups were age-, sex-, race-, ethnicity- and region-matched.
Lyme disease diagnoses identified in the Medicare fee-for-service data were compared with the confirmed and probable cases among individuals aged 65 years and above obtained through national surveillance. However, the study also notes certain limitations, such as slight differences between the Medicare fee-for-service population and the U.S. Census population regarding race, ethnicity, and sex. These differences, though small, were stable throughout the study period.
Important observations
The Medicare fee-for-service population included in the study was estimated to have a median of 17,872,466 person-years during the study period, as compared to the US Census population of 51,561,372 individuals aged 65 years and above. Person-years refer to the number of years for which persons contribute data.
The proportion of individuals from neighboring high-incidence states was higher in the Medicare population than in the US Census population.
Incidence of Lyme disease
A total of 88,485 Lyme disease cases were identified in the Medicare population during the 2016-2019 study period. This corresponded to an average incidence of 123.5 diagnoses per 100,000 person-years.
The total number of Lyme disease cases reported through public health surveillance during the same period was 34,183. This corresponded to an average incidence of 16.6 cases per 100,000 persons.
Approximately 82% of Lyme disease cases were identified among individuals residing in high-incidence states. The median incidence of Lyme disease diagnoses was 346.9 per 100,000 person-years among residents of high-incidence states, 35.3 per 100,000 person-years among residents of states or jurisdictions neighboring high-incidence states, and 29.4 per 100,000 person-years among residents of low-incidence states.
Public health surveillance data revealed that about 93% of Lyme disease cases were among residents of high-incidence states. The median incidence of these cases was 57.1 per 100,000 persons among residents of high-incidence states, 3.6 per 100,000 persons among residents of states or jurisdictions neighboring high-incidence states, and 0.6 per 100,000 persons among residents of low-incidence states.
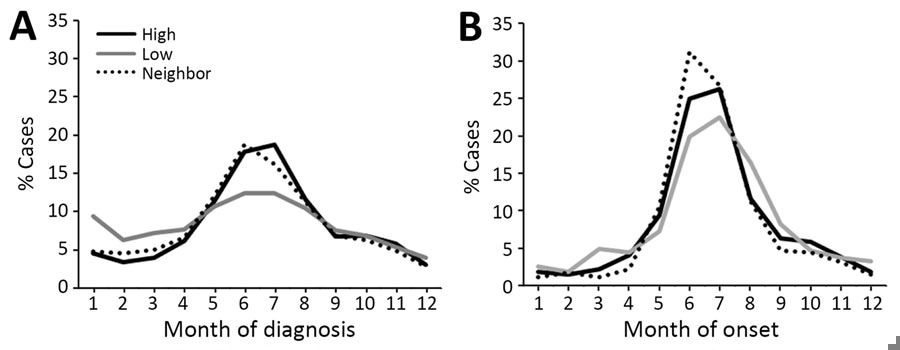
The majority of Lyme disease diagnoses occurred in the summer months. Among residents of low-incidence states, a large proportion of disease diagnoses occurred in winter months.
According to Medicare and surveillance data, the majority of Lyme disease cases were identified among men. In high-incidence states, men had the highest incidence of Lyme disease for all age groups. In low-incidence states, women had a slightly higher incidence than men only in the 65–69-year age group and 75–79-year age group.
Study significance
The study identified more than 88,000 adults aged 65 years and above diagnosed and treated with Lyme disease during 2016 – 2019 in the United States. Most Lyme disease cases have been identified among residents of high-incidence states.
The study reports a 7-fold higher incidence of Lyme disease diagnoses compared to that reported through public health surveillance. These findings are similar to the findings reported in previous claims analyses. The study also acknowledges the issue of overdiagnosis, which may partly explain the differences observed between the Medicare data and public health surveillance data. Overdiagnosis has been reported in other analyses and may contribute to the higher incidence rates observed in this older population.
A variation in Lyme disease seasonality has been observed when Medicare fee-for-service data is compared with surveillance data. Some differences in gender-specific disease susceptibility have also been observed when this study is compared with previous claims analyses.
In previous claims analyses, male children have shown higher susceptibility to Lyme disease in both high- and low-incidence states. In contrast, male older adults have shown higher susceptibility in high-incidence states.
Overall, the study findings add insight into Lyme disease patterns unique to this older population in the United States.