Decontaminating equipment and facilities has become routine in Biological Select Agent and Toxin (BSAT) laboratories. Area remediation and contamination control are essential for worker safety, research quality, and facility maintenance.
Routine vaporous hydrogen peroxide (VHP) decontamination effectively manages possible contamination in critical conditions alongside the manual removal of bioburden but requires a 35 % H2O2 starting solution. This makes it hazardous and difficult to transport.
VHP is also vulnerable to humidity and temperature. Constant exposure can trigger material compatibility concerns. The exposure cycles for VHP against biological contaminants are also laborious, between 8–16 hours of exposure time.
The TOMI SteraMist® system with Binary Ionization Technology (BIT™) was manufactured for the Defense Advanced Research Projects Agency and authorized for employment against bacterial spores.
BIT passes 7.8 % hydrogen peroxide through a cold plasma arc to quickly produce reactive oxygen species (OH radicals) approximately 0.05 μm in particle size. This size enables the vapors to work like gas and efficiently decontaminate small areas.
The test aimed to determine if iHP could contaminate biological toxins faster than VHP. The toxoids examined included ricin A chain toxoid, Staphylococcus enterotoxin B toxoid (SEB), and Clostridium botulinum A toxoid. The materials investigated were polycarbonate Lexan and stainless steel.
The toxoids were examined over various time points to verify the time required for successful decontamination as determined by testing via electrochemiluminescence (ECL) utilizing the Meso Scale Diagnostics (MSD) Sector PR2 tool.
Materials and methods
Toxoids
Ricin A chain toxoid and SEB were acquired from Toxin Technology, Inc. (Sarasota, FL). Clostridium botulinum A toxin complex toxoid (Bot) was acquired from Metabiologics, Inc. (Madison, WI).
TOMI SteraMist BIT Solution, TOMI Environmental Solutions, Incorporated SteraMist BIT Solution is intended as a hospital-healthcare disinfectant for bacteria, bacterial and mold spores, and viruses.
It is a liquid with less than 8 % hydrogen peroxide and kept in a bottle fitted to the SteraMist system.
TOMI SteraMist Select Surface Unit
The SteraMist Select Surface Unit (Product # HHA-102-02-110- SS) is a compatible, ruggedized decontamination system for biological remediation by direct spray application and small-space timed custom fogging. It measures around 25 x 22 x 15” and weighs 49 lbs.
Test coupons
Two military-relevant coupon types (polycarbonate and stainless steel) were employed during testing. The ISO 17025-accredited CBC Engineering Directorate (Aberdeen Proving Ground, MD) assembled all coupon materials.
Coupon dimensions were 5 x 2 x 0.3 cm (10 cm2 surface area). Three coupon test replicates were produced for each test run alongside test controls.
Coupon contamination
The coupons were positioned on a disposable assay mat in a Class IIA2 biosafety cabinet (BSC). The BSC interior dimensions are around 70 x 24 x 28” (LxWxH) (approx. 27 ft3).
Each coupon was contaminated with toxoid at 100 ng/ml target concentration densities for ricin A chain toxoid, 200 ng/ml for SEB toxoid, and 100 ng/ml for Bot toxoid. Five specific 10 µL aliquots (50 µL total) of toxoid were placed on the coupon surfaces and dried at ambient conditions inside the BSC.
After the last coupon in the sample set finished drying, that time was recorded as the official drying time for that set. Individual dry times for the coupons were not assessed. Environmental temperature, humidity, and coupon dry time were noted for each experiment.
Coupon decontamination, extraction, and analysis
Once the coupons dried, the BSC’s blower was turned off, an oscillating fan was positioned inside, and plastic sheeting and chemical-resistant painter’s tape were utilized to seal the BSC.
The SteraMist nozzle was positioned at one end of the hood and the spray was aimed toward the opposite corner. The SteraMist unit was set to a cycle of a 5-minute iHP injection at an 8.3 ml/min rate and then a 10-minute hold (dwell)—this 15-minute cycle equals one exposure cycle.
The amount of exposure cycle runs depended on the decontamination time point under evaluation. Time points were 15 minutes, 30 minutes, 1 hour, 2 hours, and 3 hours. After completing the final cycle, the blower was initiated, and the BSC was authorized to clear it before removing the plastic sheeting.
All coupons were lifted with sterile forceps and transported to a 50 ml polypropylene conical tube containing 20 ml PBS with 0.1 % Triton X-100. The extraction tubes were put into a large area vortex mixer (Vortex Genie) and vortexed at 950 rpm for 20 minutes. Directly following vortexing, the samples were examined by ECL using the MSD Sector PR2.
Results
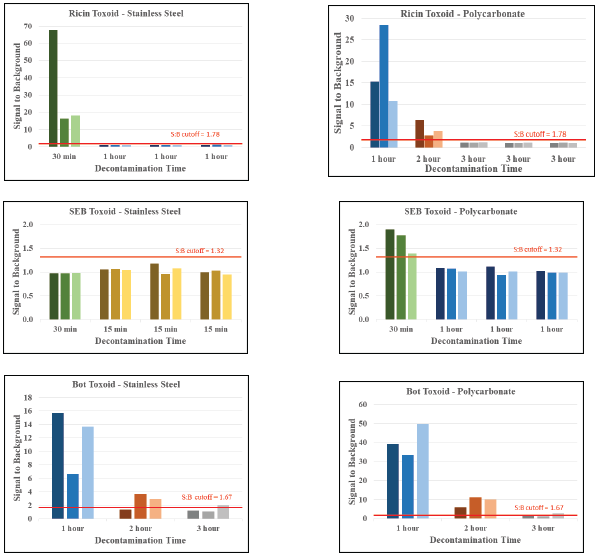
Image Credit: SteraMist Disinfection and Decontamination Technology
Conclusions
This study proved that iHP is beneficial for decontaminating biological toxoids. Decontamination times were confirmed under DoD BSAT Biorisk Program Office guidelines by running the chosen time point for each toxoid on a particular surface on three separate days.
Results indicate that iHP may more quickly decontaminate ricin than VHP. No material degradation was noted during testing on test surfaces or within the BSC, including an oscillating fan inside the BSC.
This study was completed using an injection rate of 1.52 ml per ft3. It remains unidentified why ricin toxoid decontamination was attained in one hour on stainless steel but needed three hours on polycarbonate.
Stainless steel could be more reactive with the iHP, causing more destruction of the toxoid. This pattern of extended times required for decontaminating polycarbonate coupons was also observed with SEB toxoid.
Although the researchers could not fully contaminate Bot toxoid, the information suggests a similar trend. More surfaces should be analyzed before deploying this system for site remediation to establish decontamination capabilities.
The findings for the Bot toxoid demonstrate that a further 30 minutes or 1 hour (a total of 3.5 or 4 hours) would reduce the signal to below background levels. Time and reagents were unavailable for continued decontamination testing.
Hood saturation was a notable concern during longer time points. iHP is most useful as a vapor, but throughout long time points, the BSC and coupons were regularly wet. Coupon saturation with moisture may impact decontamination effectiveness by stopping ROS (-OH) from cooperating with toxoids on the coupons.
Following the last exposure cycle, more drying time was needed before initiating coupon extraction. This study employed toxoids in place of toxins to lower the risk for initial study validation and proof of concept. This study should ideally be replicated using active toxins to verify inactivation time points.
This study utilized ECL to establish toxoid presence. ECL is a semi-quantitative antibody-based assay that will not verify toxin activity.
iHP decontamination utilizing the TOMI SteraMist device appears favorable for quicker biological toxin remediation. Until the tool is fully certified with functional toxins on various surfaces, operators should resume targeted and randomized surface sampling for the concerned contaminant to verify full site remediation.
Table 1. Summary of decontamination times for each coupon type. Source: SteraMist Disinfection and Decontamination Technology
| Target |
Coupon |
Decontamination Time |
| Ricin |
SS |
1 hr |
| Ricin |
PC |
3 hr |
| SEB |
SS |
15 min |
| SEB |
PC |
1 hr |
| Bot |
SS> |
3 hr* |
| Bot |
PC |
>3 hr* |
*Note that the Bot on SS and PC are not validated time points.
Acknowledgments
The Scientific Gaps in Biorisk Research Program funded this effort.
About SteraMist Disinfection and Decontamination Technology
SteraMist is a global line of powerful disinfection and decontamination products and services that utilizes patented ionized Hydrogen Peroxide (iHP) technology.
Our scientific expertise, innovation, and dedication to creating a safer world through cutting-edge iHP technology allow SteraMist to serve our customers and industries with trusted products, leading to a smarter way to decontaminate and control infectious diseases.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.