There has been a great deal of research into the link between gut microbiome and immunity, as well as external factors such as diet and environment, all of which have an impact on the microbiome.
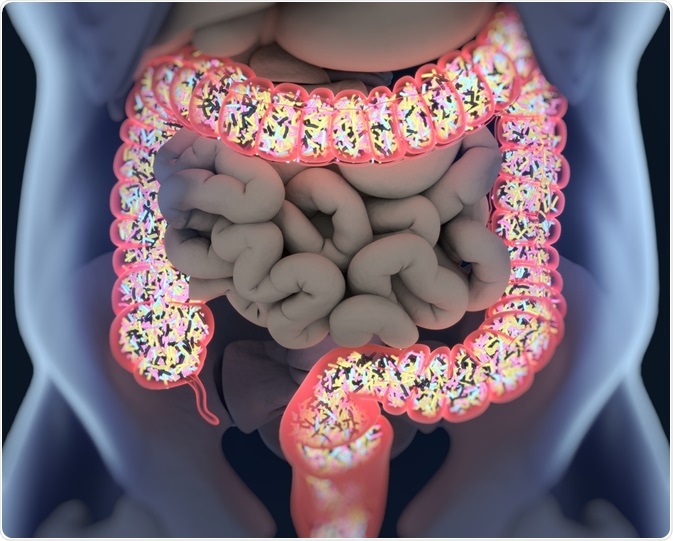
Image Credit:Shutterstock/AnatomyImage
The role of the immune system
The immune system is an extensive network of cells and biological processes that protects against infection and helps repair damaged tissue in the body. It is also key to maintaining metabolic homeostasis and is heavily integrated into the body’s metabolic pathways.
The immune system is present in all organs, it has extensive sensory capabilities, and it possesses a vast repertoire of different molecules used for communication and as effector functions. Most importantly, the immune system has the ability to learn, adapt and remember – the underlying factor in the function of vaccinations.
There are many different cells within the innate immune system and the adaptive immune system. These cells must collaborate to orchestrate a combined immune response to a given threat or exposure.
The microbiome’s contribution
The microbiome plays an important role in regulating and directing the immune response of the host. The microbiome’s role is significant because at least half the cells in the body are microbes that produce metabolites that interact with the host body’s systems, for example, supporting the digestion of food.
The microbiome’s bacterial communities are highly dependent on an individual’s diet. Fundamentally, an individual who consumes a varied diet that changes over time will develop a robust and diverse immune response, as each foodstuff entering the digestive system will require a specific series of bacteria to digest this.
Should a person stop eating a certain type of food, the respective bacteria decrease in number, but a small population will generally remain in the gastrointestinal tract.
These changes can be challenging for the immune system because each food type must be accommodated and responded to appropriately. There are different antigens (‘danger signals’) associated with the microbes that utilize the foods, as well as the foods themselves.
The immune system must recognize and respond to these in an appropriate, typically non-aggressive manner while developing an effective and balanced response over time.
Diversity in the microbiome is important as the presence of more than one microbe able to metabolize a specific food type ensures a buffer or functional redundancy. This is important in maintaining host metabolism as well as immune system development and protection.
Reductions in microbiome diversity
A reduction in the diversity of food consumed and/or a reduction in the diversity of the microbiome essentially leads to a loss of antigen exposures and tolerance adjuvants (tolerance inducing signals). Missing some of these microbes or tolerance-associated metabolites can cause issues in the immune system.
Throughout human evolution, the immune system has been hardwired to respond to these tolerance-inducing signals. If the immune system does not ‘know’ how to respond to these signals, this can result in an over-reactive immune response which can cause inflammation.
Recent studies have shown that there is a decrease in microbiome diversity, particularly when comparing changes in post-industrialized populations with pre-industrialized populations. Microbes that are important for inducing immune-regulatory responses have potentially been lost.
Improving microbiome diversity to enhance immune responses
The recognition that many people are missing some of the microbes, molecules or metabolites responsible for regulating the immune system has led to research into identifying and replacing these microbes and molecules.
This work is especially important in managing allergies, asthma and other immune system-mediated diseases. For example, an allergy is essentially an inappropriate immune response to an exogenous trigger - something outside the body that does not typically warrant an aggressive immune response, such as pollen or a particular food.
This is essentially a breakdown in immune tolerance. Research has shown that the gut, skin or lung microbiome is different in people with conditions such as food allergies, atopic dermatitis or asthma, respectively. This is the case even without the presence of disease symptoms.
Human beings are born relatively sterile instead of acquiring microbes and developing a microbiome over the first few years of life. Microbiome acquisition and community development occur in many ways beyond the natural maturation of the host immune system, for example, as a result of environmental factors such as exposure to animals, green spaces or other people.
Diet is incredibly important and is an area where it is possible to help microbiome diversity. There has been a great deal of interest in the role of non-digestible dietary fibers. Specific microbes in the colon digest these, ferment them and generate a range of metabolites.
Research has thus far focused on short-chain fatty acids, including butyrate, propionate and acetate, but the microbiome generates many different metabolites following digestion of food or dietary components.
There is evidence to suggest that levels of short-chain fatty acids early in life could be associated with protection from allergies later in life.
After making a number of models to establish how these short-chain fatty acids might be working, we discovered a potent induction of T regulatory cells, which are important for protection against atopic sensitization, asthma and food allergies.
For example, a diet featuring yogurt, fruits and vegetables early in life leads to microbiome fermentation, which generates short-chain fatty acids and improves immune regulation, helping protect against allergic sensitization.
Other dietary or health factors such as obesity can impact immune responses. For example, a poor diet with a lack of fiber and excess fat has been shown to significantly impact the microbiome, potentially leading to higher levels of systemic inflammation.
Summary and future developments
Microbiome and diet are very important in terms of their effects on immune-system function regulation. The concept of ‘healthy foods’ from a microbiome perspective includes foods that are richer in non-digestible fibers.
These are essentially food for the microbiome, helping to increase the diversity of the cells and bacteria, as well as the diversity of the metabolites reaching the immune system that are driving immune tolerance and immune functions.
Overall, non-human-encoded factors are potentially much more important for training the immune system and physiology than any human-encoded factors.
From a research perspective, it is important to identify the molecular signals that underpin and trigger immune system responses, leveraging this information to potentially reverse, prevent and treat immune-mediated diseases.
Dietary factors are key to maintaining microbiome diversity and ensuring a robust and appropriate immune response. Current approaches to managing this includes microbes in the form of probiotics, or prebiotics, isolated components, postbiotics, or metabolites to help manage and improve this.
Ongoing work into developing and using combinations of all of these approaches will continue to be key, with expertly delivered clinical studies from trusted organizations such as Atlantia Clinical Trials likely to be central to formally proving the efficacy of these interventions.
About Atlantia Clinical Trials
Atlantia Clinical Trials Ltd is a CRO that specializes in conducting studies in foods, beverages and supplements for companies world-wide that want to scientifically validate their functional ingredients to support an: EFSA (European Food Safety Authority) Health Claim; FDA (Food & Drug Administration) Structure Function Claim; or General Product Marketing Claim.
Atlantia works with world leading scientists (among the top cited 1% internationally, in the areas of digestive health and functional foods) at the: APC Microbiome Institute in University College Cork, Ireland; Teagasc, Moorepark, Ireland and recognized centers of excellence globally.
Atlantia runs and operates its own clinic sites and conducts all studies to ICH-GCP standard (International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use - Good Clinical Practice). Its team includes physician experts in digestive health, mental health (psychological stress and cognition), cardiovascular health, sports performance, metabolic disease, bone health, immune health and healthy ageing. The clinical team also includes project managers, research nurses, nutritionists, certified sports trainers and lab researchers.
Atlantia manages all elements from protocol design, placebo manufacture, recruitment, and study execution, to sample and data analysis, statistics and report/dossier preparation to provide a service which is technically, scientifically and clinically superior.
The clinical studies cover a broad spectrum of functional food and beverage categories, such as dairy, cereal, probiotic, different protein forms, infant-specific foods, vitamins/minerals, plant or marine extracts and medical foods.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.