The mTOR pathway is probably the main pathway in humans and other animals that drives growth. That is, the accumulation of mass and adding mass to make an organism bigger by both making more cells, and making cells grow and become bigger.
The mTOR pathway ties that process to whether we have nutrients in our environment. It's one of the key systems for an organism to adapt its physiology to the nutritional state and for almost every tissue that has been looked at, there's a connection between mTOR and the physiology of that tissue.
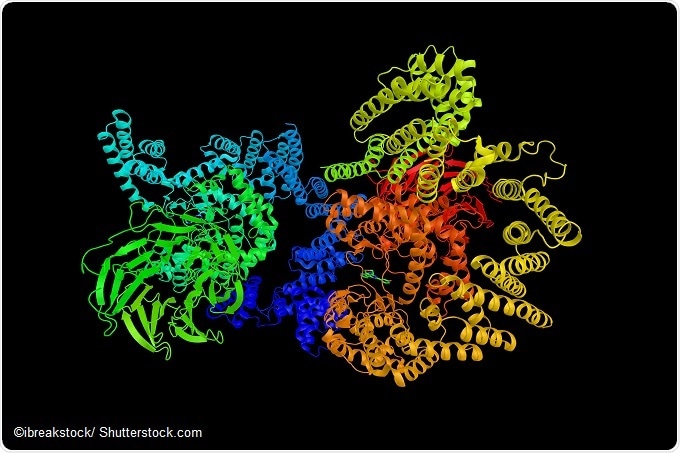
The way it was discovered was through studies into an immunosuppressant drug that we now know has a variety of other effects, and it was purified as directly binding to the mTOR protein, which is a kinase.
How is mTOR regulation and dysregulation thought to affect normal and diseased physiology?
There's evidence that both too much mTOR activity and too little mTOR activity is a problem and it happens in different diseases.
For example, too much mTOR activity is clearly connected to certain types of cancers and neurological diseases, particularly epilepsy and there's some evidence even for autism. Too little mTOR activity is connected to diseases such as atrophy of the muscle in certain situations, even aging a certain cell.
However, what is less well understood, is why those changes in mTOR activity have those effects. There are some big processes downstream of mTOR like autophagy which is our self-eating, as well as protein synthesis that is regulated by it, which are likely interconnected to all these diseases.
In what ways has your research helped to advance our understanding of the mTOR pathway over recent years?
We've been studying this pathway for a long time, as we first discovered mTOR when I was a student. Over the years we've started with mTOR as the focal point and then built outwards.
We initially identified two protein complexes, which we now call mTOR complex 1 and mTOR complex 2. The better-known complex is mTOR 1, and it is this one that’s connected to some of the diseases I mentioned before. Once we had those complexes, we went out and found regulators of those, and regulators of the regulators.
What I think has been our most important contribution over the years is identifying most of the components of the pathway. There's probably 30 proteins or so that we've identified that we can now say are part of this system and we've helped to push that and to do that work.
Another aspect is that we've tied an organelle called the lysosome, a degradative organelle, to the regulation of this pathway and that conceptually was interesting from a point of that this particular organelle is very important in the regulation of this pathway which is involving growth control.
One of the interesting aspects of our mTOR work is that we're directly connecting nutrients that come from the outside largely to the regulation of this major pathway by finding the proteins are actually the sensors of nutrients. I think that has been an important step that we've taken in the sense that we have proteins that directly combine nutrients. In a way, you're connecting outside world directly to the regulation of the system really without any intermediates.
What impact does caloric restriction have on cellular aging?
Caloric restriction means lowering the amount of calories ingested, to not a malnutrition state but to normal calories a normal organism would eat if given free access to food, has life span extension effects. At the organismal level, it is quite clear that this is true, particularly for animals that we have captive data for and we can do this with.
If you take a cell from an animal that has been caloric restricted versus one that wasn't, exactly what is different in those cells is harder to know. It is quite clear that one of the things that happens is inhibition of the mTOR pathway and that has been shown through genetic studies to be important for the effects of caloric restrictions.
It gets back to the question that we talked about earlier. What is it that mTOR is regulating that is important there? And people disagree about what those might be. My view is that the reason that manipulation of the mTOR has these life span depending cycles is that mTOR does so many things.
The way I like to put it is, if you think about renovating an old building and making it a modern building, you have a general contractor that has plumbers, electricians, carpenters etc. and none of those by themselves would be able to renovate that building. So mTOR, by being this master regulator, allows many things from the cell to be fixed.
Do you think it would be possible one day to manipulate the mTOR pathway to protect against age-related diseases such as cancer and diabetes?
There are drugs that manipulate this pathway and they're certainly used clinically and there are still clinical trials being done looking at aging related physiology, for example, aging of the immune system. I think the answer is yes, that that's already happening.
The real question is whether the potential side effects of manipulating mTOR will be tolerated versus the potential beneficial effects. I think that is still an open question and it's going to very much depend on the dose that someone is going to have to use. Certainly, at the dose used for some of the clinical applications, for example immunosuppression, that's going to be too much. It has too many side effects for us to tolerate that for an anti-aging related disease application.
Many people believe that much lower doses are going to be beneficial and if that turns out to be the case, and I think there may be some evidence that that's true, I think these molecules will be used to slow the appearance of aging-related diseases.
What will be the main challenges to overcome?
The main challenges are that too much mTOR is bad and too little mTOR is bad. It’s difficult to find a happy medium, and so being able to use drugs to get to that happy medium is the challenge.
We may find that different tissues have different preferred amounts of mTOR. If the liver tolerates a certain amount of mTOR but another tissue tolerates less, this could be problematic.
Can you please outline the new type of microarray and image analysis software your lab developed to identify the role of genes inside cells? What impact has this had?
Early on in the lab, we developed systems where we could print perturbagens. When perturbagens got in the cells, they could perturb gene function, and then we could put cells on top of those - so we had microarrays for example, of CDNAs, that would get into cells and be expressed. The concept was to print perturbagens on a surface and then grow cells on top of that surface, and then we develop tools to do image analysis of the cells that were there.
I think these have had less of an impact than our work on mTOR and the reason for that is simply that people started doing screens in different ways. Pool screening, where everything is mixed together and we have bar codes that we can use to follow the cell, I think that's become less important, certainly for us and for the community in general. However, there was a time when they were used.
What further research is needed to increase our understanding of the role of the mTOR pathway in growth control and nutrient sensing?
I think one of the big challenges we have now is that we've identified many of the pieces and we've done most of that in cells and culture. Now going from that to what actually matters in each different tissue and each different cell of those tissues under many different physiological situations and how we can manipulate that, potentially for benefit, is a big challenge.
This is because, what we have found is all the components of the system, or many different components but how exactly they're used under different situations is not so clear in vivo and probably exceedingly complicated. To figure that out, we need to go from our nice tissue culture systems, to the messy but incredibly interesting physiology that happens in vivo.
Where can readers find more information?
Sabatini lab, Whitehead Insititute
About Dr. David M. Sabatini, M.D./Ph.D
 David M. Sabatini is a Member of the Whitehead Institute for Biomedical Research, Professor of Biology at the Massachusetts Institute of Technology, and an Investigator of the Howard Hughes Medical Institute. He is also a Senior Associate Member at The Broad Institute MIT and Member of the Koch Institute for Integrative Cancer Research at MIT.
David M. Sabatini is a Member of the Whitehead Institute for Biomedical Research, Professor of Biology at the Massachusetts Institute of Technology, and an Investigator of the Howard Hughes Medical Institute. He is also a Senior Associate Member at The Broad Institute MIT and Member of the Koch Institute for Integrative Cancer Research at MIT.
David’s lab studies the mechanisms that regulate physiological and pathological growth and metabolism in mammals and also develops new technologies that can be applied to diverse biological problems. A longtime interest of the lab is the signaling pathway anchored by the mTOR kinase, which David discovered when he was an M.D./Ph.D. student at Johns Hopkins Medical School.
The mTOR signaling network is a central regulator of growth, metabolism, and aging; the target of the well-known drug rapamycin; and is deregulated in common diseases, including cancer and diabetes. Work in David’s lab has led to the identification of most of the established components of the pathway, including the mTORC1 and mTORC2 complexes, and to an understanding of their cellular and organismal functions.
In recent years the lab has discovered the amino acid sensors and signaling molecules that convey amino acid sufficiency to mTORC1. The discovery of the Rag-Ragulator complex as a lysosome-associated machine that signals amino acid levels to mTORC1 revealed a key role for the lysosome in nutrient-sensing. His identification of rapamycin-resistant functions of mTORC1 and mTORC2 prompted the development of a new class of compounds that inhibit both and are now in clinical trials as anti-cancer agents.
In work in vivo, David’s lab uncovered molecular mechanisms through which fasting/feeding regulate organ physiology, including hepatic ketogenesis and intestinal stem cell self-renewal, as well as tumor growth. David is also interested in how small molecule metabolism affects growth control and has studied the role of the serine synthesis pathway in cancer and used genetic screens to find that aspartate synthesis is an essential function of mitochondria in cell proliferation.
David is also active in technology development, creating methods for purifying unstable protein complexes, cell-based microarrays for high throughput screening of cDNAs, and genome-scale RNAi and CRISPR/Cas9 libraries that are widely used.
David received his B.S. from Brown University magna cum laude and his M.D./Ph.D. from Johns Hopkins University in 1997. He completed his thesis work in the lab of Dr. Solomon H. Snyder in the Department of Neuroscience. Later in the same year, David was appointed a Whitehead Fellow at the Whitehead Institute for Biomedical Research. This was followed in 2002 by a dual appointment as a Member at the Whitehead Institute and Assistant Professor of Biology at the Massachusetts Institute of Technology.
David has received a number of distinctions, including being named a W. M. Keck Foundation Distinguished Young Scholar, a Pew Scholar, a TR100 Innovator, a recipient of the 2009 Paul Marks Prize for Cancer Research, 2012 The Earl and Thressa Stadtman Scholar Award from ASBMB, 2013 Feodor Lynen Award from Nature, the 2014 NAS Award in Molecular Biology, the 2014 Colin Thomson Memorial Medal, and the 2015 Glenn/AFAR Breakthroughs in Gerontology Award. David Sabatini most recently became a member of the National Academy of Sciences. He is also the 2017 recipient of the FNIH’s Lurie Prize in Biomedical Sciences.