‘Biomarkers’, short for ‘biological markers’ are essentially something that is taken out of the body, for example fluids or tumor tissue, which is used to give you an idea of a biological process, either normal or abnormal.
Biomarkers fall into different categories: diagnostic biomarkers, are used to identify a disease; prognostic biomarkers, help clinicians to determine, for example, whether you're more likely to die or have problems with a disease; and there are some that can be used to inform treatment, to determine whether one therapy would be more successful than another.
Biomarkers and Biomarker Testing - An Overview for Colorectal Cancer Patients
The biomarker concept has been around for a long time, but what has been lagging is getting them into the clinic. There’s been more excitement surrounding them recently because there are starting to be the biomarkers used in clinical care, which starts leading us towards a very attractive goal in medicine, personalized or precision medicine.
Why is clinical implementation of biomarkers so important?
Medicine traditionally has been very hit or miss. You see a patient and make a diagnosis and you try a medication. Maybe they'll have a side effect, maybe it'll work, maybe it won't work. If it's not effective or they're having side effects then you try another medicine and repeat the process.
Finding something biological that might help healthcare professionals decide how to treat patients, may help avoid giving medications to patients that are not going to work or be less effective than others.
It's been a dream in medicine but it's not started to materialize until relatively recently. That's why there's a lot more excitement. It's also why there hasn’t been as much education on biomarkers aimed at general audiences.
Colorectal cancer is one area where we already have biomarkers that exist and can help with both the prognosis as well as that can help guide therapy.
Can you give an example of a biomarker that is currently used during the diagnosis and prognosis of colorectal cancer and how that may affect diagnosis and treatment?
Typically, what will happen is if somebody presents with colorectal cancer, they may have symptoms, they may see blood in their stood, abdominal pain, weight loss, or they may be having a routine colonoscopy and colon cancer is diagnosed.
To make the diagnosis, typically the tissue will be obtained and the pathologist will look at it. They might see changes in the tissue that suggest that it's cancer. Since now they have this tissue, they can run tests for certain biomarkers.
There are several different ones that the pathologist can use, one that’s commonly used for colorectal cancer now, used regardless of the stage is related to micro satellite instability. This is related to DNA repair.
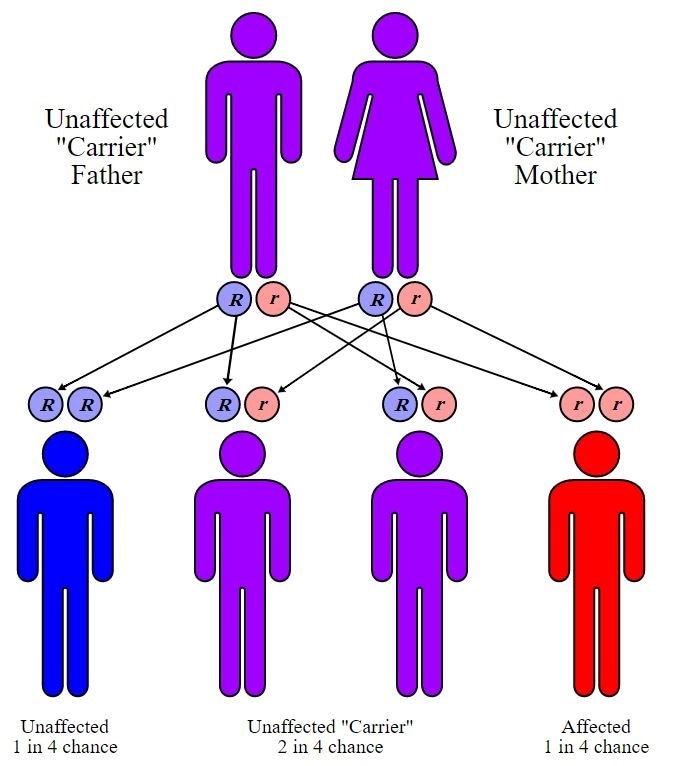
You have certain genes in your body that are involved in repairing DNA errors. Your DNA is always replicating, and of course like anything, it's not 100% accurate so it’ll make mistakes. When these mistakes come, these genes go ahead and remove them.
In some hereditary colorectal cancer syndromes, where multiple members of the family can have it, these genes aren't working properly. We can determine that by looking at the tumor tissue, where you can see too many DNA mistakes. That's called a micro satellite instable high.
The reason this is important is that tumors with a micro satellite instable high are often associated with a diagnosis of Lynch Syndrome. We know that if you have this type of cancer, you actually have a better prognosis, so this is a biomarker that can inform prognosis, these individuals tend to do better.
There is some data to suggest that if you have these types of tumors that you may respond more to a new type of therapy called checkpoint inhibitors, a cancer immune therapy. While, there's also some data to suggest that some of the traditional chemotherapy we use in colorectal cancer, called 5FU, may not be as effective.
How can biomarker testing affect those that are at risk of developing hereditary colorectal cancer?
Seeing these mutations and multiple cases of colorectal cancer in the family may lead you to identify families that may have Lynch Syndrome, which can have important implications on how other asymptomatic family members, who don't have a diagnosis, are screened. We'll screen them more aggressively and we'll look for other cancers that follow into it.
© CBurnett
How has cancer research affected research into new biomarkers?
We've learned a lot from cancer research, we know that there are a relatively well conserved set of genes that seem to be mutated consistently across all colorectal cancers. Sometimes we call these driver mutations. These we see repeatedly in different colorectal cancers. We know that the mutations of these genes tend to affect the signaling pathways that help drive the cancers.
There's a mutation in the RAS family, which is either KRAS or NRAS, where we know that when patients have mutations in certain specific areas of the proteins, they may not respond to some of the chemotherapy that we use.
That's useful information because we try not to expose patients to with toxicities where we don't think they're going to have a benefit.
The chemotherapy in this situation is a chemotherapy that blocks a pathway called the epidermal growth factor receptor, which is a pathway in the body that helps stimulate cells to grow.
Other mutations, on a gene called BRAF, are similar to KRAS, if you have this mutation, you may have a worse prognosis. The cancer may be more aggressive and you may not have as much of a response to these same type therapies.
What's even more exciting is that there are a wealth of other biomarkers that are being identified that are still in the research stage. Through research you identify what biological pathways are not working correctly in cancer and then through this, you can engineer therapeutic antibodies that may shut off or turn on a pathway.
What you're doing is you're targeting your treatment directly to the pathway. The biomarkers are coming hand in hand with the therapies to find something that will work specifically for the specific tumor. Different tumors will have different mutations that might be driving it.
There's a lot of excitement in that as this field continues to develop. We already have some early biomarkers that are clinically developed, but as more get into clinical medicine we will have a lot stronger rationale for the therapies that we use.
It will be hopefully more efficacious and at the same sense safer, but a lot of this research is still ongoing and although there have been hundreds of different biomarkers that are being investigated right now, we still only have a small subset that are actually in clinical practice.
How different are biomarkers for individual patients? What can the differences between these biomarkers indicate for patients and their colorectal cancer characteristics?
As medicine gets more and more personalized, we might get to a point where you have a very specific set of biomarkers for every individual. There's some thought that there are unique mutations that occur in tumors that are maybe more specific for each individual tumor.
Right now, in terms of therapies, we look for pathways and a treatment that will work for a subset of issues. We have known mutations that are relatively common, for instance, almost half of colorectal cancers have the KRAS mutations, then we can look for more specific mutations.
It is easier to test for them too because these genes themselves are very, very long and to identify every mutation in a gene usually requires next generation sequencing, which can be very expensive.
If we can target certain regions where we see these mutations and know that these mutations may affect prognosis, you can hone in on that. Individually one patient may have this mutation and one patient may not, but on a population basis, you can expect to have a reasonable subset that will have the same mutation.
However, even in KRAS and BRAF mutation, there may be other mutations in the gene that might not have the same effect of the main ones that we've been interested in.
When should patients be tested for cancer biomarkers?
We would usually say that almost anybody who has colorectal cancer, either diagnosed at a younger age or in certain locations in the colon with multiple family members affected, will want to be tested for biomarkers related to this micro satellite instability.
For the therapy related to the epidermal growth factor receptor, those are usually reserved to more advanced cases. It's generally recommended that we test individuals who have cancer that is more advanced than just metastatic.
Of course, you'd want to test from the onset. You'd already have the tumor tissue and because it could guide therapy you'd want to do it at the very beginning. This would be early in the course.
That has a lot to do with the impetus with the Biomarked campaign, Fight Colorectal Cancer's campaign to help get more of this information and educational material out to a general audience because you want patients to be informed of the processes, and like most new findings in medicine they take a good while to diffuse.
This is also true of doctors too, who may take a while to receive the latest information. To help speed this up, it makes sense to try to engage patients and have them act as their own advocate, to bring this information to the conversation, because there likely are healthcare professionals and centers who aren't routinely testing for these biomarkers while others may.
Patients who are more informed are more likely to ask about these tests and ask for these tests to be completed.
Would you also test family members for the same biomarkers?
Yes. For family members, the only way to test them when they are without symptoms is for biomarkers related to that cancer such as micro satellite instability. For example, if a patient had Lynch Syndrome, the physician will usually have identified a specific mutation in the patient who has the cancer, then you can look for that in their family members.
Alternatively, you can increase their screening or use the typical screening procedures that you would use in families that are at high risk to begin with.
We tend to try to reserve biomarker identifications for if we have found a specific mutation in a patient with what looks like a family syndrome. Then we look for that in other family members. That will be DNA and is what is call a germ line. That's a little bit different from the mutation specifically in the tumor and that can be measured in blood.
How are biomarkers tested for in cancer patients?
The most common method is via the tumor tissue itself. What you're looking for is specific mutations in the tumor as the cancer is growing, as it's going to have additional mutations.
Certain mutations are going help select out clones, which will help, as a lot of these tumor cells will look the same. That's what you're going to initially test for, looking for some of these mutations.
There are also blood biomarkers. One example are biomarkers of recurrence, there's a blood biomarker called CEA, which we will test on individuals who have been diagnosed with cancer both before and after a treatment such as a surgery.
After surgery, the levels of these biomarkers will typically go down and if you see an increase over the next couple of months, then it may suggest that there might be a recurrence of that cancer.
In the colorectal cancer setting, that's probably the most common blood biomarker. Healthcare professionals are looking to trying to capture circulating tumor DNA.
These are generally more research based, but may eventually become something informative to help identify the needle in the haystack, relating to DNA that signifies a tumor as opposed to their own DNA in the bloodstream.
Then you could learn about the genetic makeup of the tumor without necessarily having to do a biopsy and take the big piece of it. Right now, most of what we do and most of what dictates clinical care has to do with taking a piece of the tissue.
Most of these tests are looking for genetic mutations. They use a test similar to PCR which looks to sequence very specific regions of the genetic code because the genome is so huge and we know can narrow the search down to specific areas where we see these mutations.
Researchers are still learning about new, unusual variants that hadn't been known before and sometimes it's hard to know what this means. We will generally know that a particular gene is involved, but that gene is very long with a lot of DNA in it.
We will know that a mutation in a particular part of the gene is concerning, but if we pick up a mutation in another part we won’t necessarily know the implications of that.
For now, a lot of research is being focused on the specific regions we already know a little bit about. As we do more studies, get more registries, we get more tumors, have more people involved in these clinical studies, we can learn more about what individual mutations might mean.
What is being done to educate people of the importance of colorectal cancer biomarkers?
Currently, not much at all, which is why I'm excited about the Biomarked campaign. Fight Colorectal Cancer is an advocacy organization which has done some really great work educating individuals.
Through engagement with stakeholders, patients and family members had realized that a lot of folks were not really sure what was going on with biomarkers, what it meant to have a biomarker and how that might be important to understand these.
Please give a brief overview of Fight Colorectal Cancer and the recent work that they have been doing.
Fight Colorectal Cancer started a campaign to produce education materials and called it Biomarked and this is really inspired from individual named Clint Cummings. He was a tattoo artist and was diagnosed with advanced colorectal cancer and unfortunately passed away six months ago.
What We Do at Fight Colorectal Cancer
He became very active in the advocacy organization and trying to promote this message. In response to that, they came up with the Biomarked campaign and they liken it to a tattoo which can be unique and individual.
The campaign has put together some great resources. On their website, they have videos of cancer survivors who have commented on how biomarkers might have impacted their therapies. They have a lot of testimonials and then they have a lot of educational material on their website about biomarkers and colorectal cancer in general.
This is both for patients, family members and providers too. It’s very useful and it will be useful for both providers as well as for patients in their families.
What does the future hold for biomarker testing? What advances do you hope to see in the near future?
As far as the biomarkers themselves, there's a lot of interest in a lot of different types of markers. Not only markers that are related to gene differences and the tumor itself, but a lot of circulating biomarkers from liquid biopsies. Researchers are also looking at gene methylation or microRNA.
It's very difficult, to evaluate and hone in on the valuable information that will move forward into applicable clinical practice. It will take a lot more studies and there is certainly a lot of interest including at the national level, from the National Institutes of Health.
Biomarkers almost routinely added, at least as an exploratory aim, to almost every clinical trial now where they'll store blood or tissue samples to look back to see if they might find a biomarker.
That might help inform how well the treatment worked or the response. I think there's a lot of work on it and I think we will probably be seeing in the next 5 to 10 years, an explosion in different biomarkers which will hopefully result in a very, very targeted treatment regimen.
Before, cancer treatment was based on chemotherapy, you knew that cancer cells were about the fastest growing cells in the body so you just gave medicines that killed fast growing cells, but there is a lot of collateral damage with that. It wasn't very specific.
Now that we have better understanding through better microbiological tools and the different pathways involved, you can target those pathways, but not everybody is going to have the same pathways involved.
It really helps to focus in on people who might benefit from these very specific targeted therapies. We've already seen some really great advances in melanoma, where there's been some therapies related to BRAF and I think we're starting to get there in colorectal cancer where now we're going to certainly have biomarkers that will help direct therapy.
I think it's moving in the right direction. I think there is a lot more advances that are probably going to have to be made and the best news is we already have things in clinics right now.
If you had called me 10 years ago, we'd say, "Oh yeah, they always talk about this. Maybe one day something will happen," but actually things are happening. It's exciting to see that.
Where can readers find more information?
https://fightcolorectalcancer.org/biomarked/
About Dr Harvey Murff
Dr Harvey Murff is an internal medicine doctor and researcher at Vanderbilt University, with interests in the prevention of colorectal cancer. Dr Murff’s research includes both clinical studies as well as observational studies investigating dietary type interventions as a way to reduce colorectal cancer. Dr Murff has completed research investigating colorectal cancer screening.