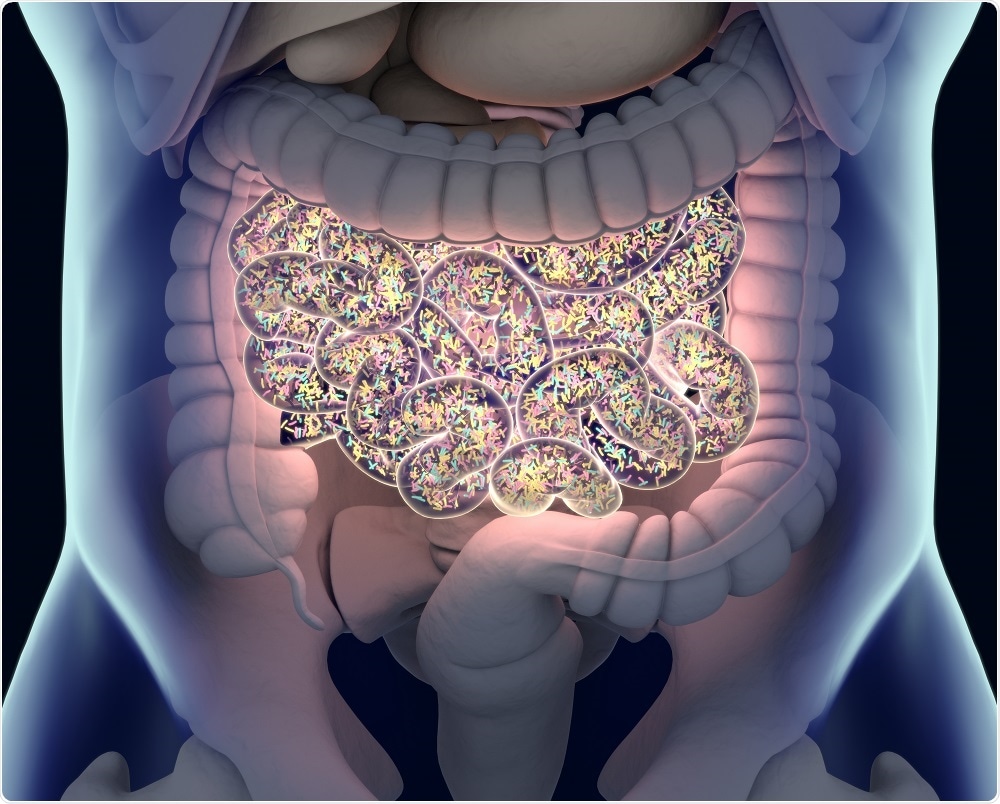
For example, Staphylococcus aureus is typically found on the skin due to the slightly acidic pH of the skin and the abundance of oxygen. In the human gut, where conditions are often anaerobic, bacteria such as Lactobacilli are found.
What is the relationship between the microbiome and good health?
Focusing on the human gut, the microbiome in health is useful for several functions, including digestion of food, protecting the intestinal barrier and engaging the local immune response. This results in a metabolic factory that can communicate with the organs of the body. Bacteria in the gut can influence organs that are near, such as the liver and the bowels but also organs that are far away, such as the brain.
What are the risk factors for cirrhosis? How are these risk factors used to guide medical intervention?
The major risk factors for cirrhosis worldwide are viral hepatitis, alcohol and fatty liver disease. Often, these conditions co-exist and go relatively unnoticed by the patient, like a silent disease. The treatment of these underlying diseases could potentially prevent the development of cirrhosis and subsequent hospitalizations, but they remain undetected for many years, the cirrhosis itself may be the main driving force behind these complications.
How common is cirrhosis-associated hospitalization? What causes patients to be hospitalized with this condition?
Cirrhosis has an asymptomatic (or compensated phase) where the liver is still able to perform all of its functions, and an advanced (or decompensated phase), where complications set in. The most common cause of cirrhosis-associated hospitalizations are complications such as fluid accumulation in the belly (ascites), confusion (hepatic encephalopathy), infections and problems with kidney function.
Patients with cirrhosis are also prone to liver cancer, which is another cause for hospitalization. Sadly, hospitalizations are distressingly common, often lead to re-hospitalizations and are very expensive regardless of the country studied.
Why is it important that new methods are developed to predict the risk of cirrhosis-associated hospitalization?
The current methods, including routine laboratory and clinical exams, have a limited predictive ability. For an outcome that is this expensive and fraught with readmissions and hospital-associated infection risks, we need to enhance these models.
We recently published a study in JCI Insight where we analyzed the microbiome of a large cohort of patients with cirrhosis. We carried out DNA and RNA analysis of stool samples provided by patients, and used this to build up a picture of the microorganisms present in their gut.
The DNA allowed us to determine the presence of live or dead bacteria, whereas the RNA demonstrated the presence of live and metabolically active bacteria. We studied the patients before and after therapies, based on whether they were on antibiotics and whether they had kidney problems or not. All patients were followed over 90 days to determine hospitalizations.
When we compared the usual clinical care models to predict hospitalizations to models that included either the DNA or RNA results, the microbiome-containing models were superior in predicting hospitalizations over and above the clinical models alone.
Importantly, the DNA+Clinical model was equivalent to the RNA+Clinical model in the prediction of hospitalization. We therefore concluded that microbiome analysis adds significantly to our current clinical models in predicting the risk of cirrhosis-associated hospitalizations.
Do you think that microbiome analysis will be routinely used in healthcare to assess the risk of cirrhosis-associated hospitalization?
It is early days yet but certainly could be an option in the future.
 Credit: Anatomy Insider/Shutterstock.com
Credit: Anatomy Insider/Shutterstock.com
Do you think that microbiome analysis could be used to predict the risk of hospitalization for other chronic conditions?
Cirrhosis is associated with a clear disturbance of the gut microbes, which is related to the liver’s proximity and integration with the gut. This certainly should be used to predict outcomes in other gut-based diseases.
What are the next steps for your research?
We have completed a multi-center analysis of outcomes during hospitalizations for patients with cirrhosis and are currently carrying out trials related to fecal microbial transplantation.
About Dr. Jasmohan Bajaj
 Dr. Jasmohan Bajaj is a Professor of Medicine in the Division of Gastroenterology, Hepatology, and Nutrition at Virginia Commonwealth University and McGuire VA Medical Center, USA. His research focusses on hepatic encephalopathy, chronic liver disease and the microbiome, areas in which he has been principal investigator or co-investigator of many clinical trials.
Dr. Jasmohan Bajaj is a Professor of Medicine in the Division of Gastroenterology, Hepatology, and Nutrition at Virginia Commonwealth University and McGuire VA Medical Center, USA. His research focusses on hepatic encephalopathy, chronic liver disease and the microbiome, areas in which he has been principal investigator or co-investigator of many clinical trials.
Dr. Bajaj is the Chairperson for the North American Consortium for Study of End-stage Liver Disease and is the current President of the International Society for Hepatic Encephalopathy and Nitrogen Metabolism.
He is also an Associate Editor for the American Journal of Gastroenterology and is on the editorial board for Journal of Hepatology, Hepatology, and Liver Transplantation.