Sponsored Content by AbcamMay 1 2020
An interview with Dr. Nicole Polinski from The Michael J. Fox Foundation for Parkinson's Research (MJFF) and Dr. Elnaz Atabakhsh from Abcam, discussing the importance of developing biomarkers for Parkinson’s and the partnership between MJFF and Abcam.
Which biomarkers are currently used for Parkinson’s disease and why are additional biomarkers needed for this condition?
Nicole: The diagnosis of Parkinson’s Disease is based on the presence of motor symptoms. Patients typically present with a tremor, or issues with balance and gait, and undergo a series of tests which determine whether the classical hallmarks of motor dysfunction are present. The disease is only truly confirmed post-mortem.
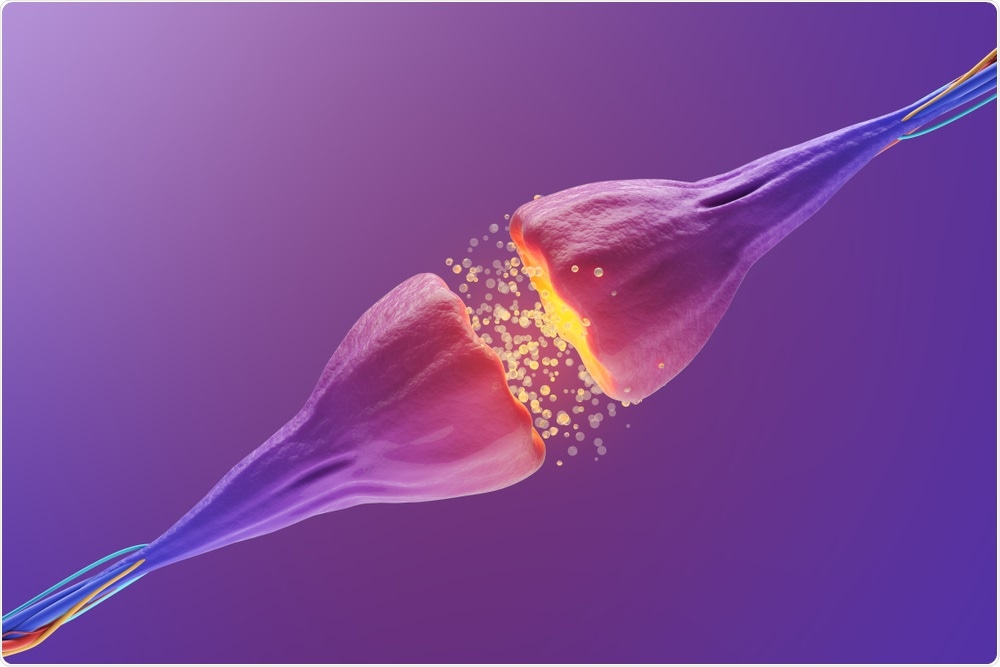 KateStudio | Shutterstock
KateStudio | Shutterstock
We do have an imaging biomarker in development; it's a scan of the brain that measures levels of dopamine transporter. What we've seen is that patients with Parkinson's have less dopamine transporter proteins than healthy controls.
So, it's a good read-out that can tell you whether you may have Parkinson’s. However, there are some patients that present with symptoms that do not have evidence of lower dopamine transporter. These patients are considered to have a separate condition.
Now, diagnosis is based on motor symptoms, and sometimes the additional brain scan, which is very expensive and therefore seldom used. This creates an issue because motor symptoms can fluctuate based on how the patient feels.
I think we've all had those circumstances where we've gone to the doctor with a problem, and then it's magically gone. It’s the same with Parkinson's disease. With such a subjective read-out, the results can differ based on the doctor you're seeing and their experience with Parkinson's among many other things.
We need a better diagnostic method for this disease that's less subjective and more stable across time, and, eventually, something that can help track disease progression.
How does neuroinflammation contribute to the pathogenesis of Parkinson’s disease? When does it appear and are there any measurable markers of neuroinflammation?
Nicole: It's still a big open question: whether neuroinflammation in Parkinson's disease contributes to the disease once it's started or whether it initially starts the disease.
We think that Parkinson's may not be one disease, but multiple. In certain cases, such as head trauma, for example, it could be possible that inflammation leads to the development of Parkinson's disease. However, in cases where there is a genetic mutation that has been linked to Parkinson’s but is not related to inflammation, we think that neuroinflammation is probably a consequence of disease progression.
Right now, we don't have really any great biomarkers for Parkinson’s, so we're testing different assays and different platforms to see if they can detect differences between Parkinson's patients and healthy controls. I think the next step will be to determine whether there are any differential immune signatures between patients or not.
It's still in very early stages; there are a lot of issues that can affect the inflammatory signature of a patient, from the time of day to exposure to different viruses like the flu, and sample collection and preparation methods.
Using models of Parkinson’s disease, we are hoping to tease out pathways, and maybe if we have a better understanding of the pathways involved in the disease, we can find something upstream or downstream that doesn’t fluctuate with time of day or other factors. We can then develop a diagnostic test that gives a better readout.
 Kateryna Kon | Shutterstock
Kateryna Kon | Shutterstock
How are the Michael J. Fox Foundation and Abcam working together to discover new biomarkers for Parkinson’s disease?
Elnaz: Abcam and The Michael J. Fox Foundation have been working together for almost ten years. The collaboration aims to develop antibodies for difficult-to-detect targets in Parkinson's disease.
More recently, Abcam and MJFF’s collaborations were expanded to our multiplex platform. The goal of this particular study was to try and determine if we can tease out some of the finer points on neuroinflammation. For example, is it chronic versus acute? Are there any gender-specific components? Can we use the serum sample as the surrogate readout for what's going on in CSF?
The research is using Abcam’s FirePlex platform, which is a multiplex assay that comprises an internal biomarker development platform and internal antibodies. This makes it a really unique tool to build exactly what’s needed.
It has been a really collaborative effort where we took feedback from the scientists at MJFF that is enabling our assay team to develop a comprehensive neuroinflammation panel.
Nicole: I would say the biggest advantage to this partnership is how collaborative it is. It was a couple of iterations and a lot of working together to refine what was already in place.
How does the FirePlex platform work?
Elnaz: FirePlex technology was developed at MIT about ten years ago using a method of photolithography to polymerize liquid PEG into bioinert particles. FirePlex started out as a multiplex nucleic acid-based detection platform and using our in-house antibody development expertise we’ve expanded into developing multiplex immunoassays as well.
Right now, we have two immunoassay options; one that's designed for screening and is run in a 384-well format in a straightforward, automatable workflow. The second is a platform is run in a 96-well plate format and is designed for biomarker discovery. These multiplexed assays are specifically designed for when you don't necessarily know what you're looking for and you want to look at a broad set of detection ranges.
The goal of the FirePlex technology is quite simple: to provide a technology platform that enables the discovery of biomarkers and for verification studies to be carried out using small sample inputs.
We know it's not possible to ask clinicians to supply hundreds of microliters or milliliters of sample for just one project when there are hundreds of projects that one specific cohort is trying to address with a finite volume of sample. Therefore, being able to support limited sample inputs and still advance biomarker studies without depleting precious samples was vital.
Being able to work directly from biofluids without sample analysis is also important because it means additional variables are not being introduced that create artifacts in the assay.
Almost all of our panels have been informed by feedback from our collaborators. We think that this is important because science doesn't happen in a vacuum but is a truly collaborative endeavor.
What have you found so far?
Elnaz: We were looking for protein and microRNA biomarkers that might help differentiate people without Parkinson’s from those with the disease. From the immunoassays, we identified some individual analytes that may be of interest.
Based on the preliminary studies, we believe that neuroinflammation could provide a good biomarker for Parkinson’s disease. We will need to further tune the panel design and make some modifications to the targets we include. We’ll also likely split the panels into high expressers and low expressers to further enhance the measurement of those analytes.
From the microRNA side, I think it's interesting that we see the enrichment of the neural-specific micro RNAs in the serum. That's a pretty good internal validation that you’re seeing some level of communication between these different matrices. We’ve yet to find out what this means.
We’re anticipating that the RNA sequencing data might help narrow down and inform a different panel design.
 ktsdesign | Shutterstock
ktsdesign | Shutterstock
How close do you think we are to producing a complete set of biomarkers that work to help diagnose and inform the treatment and prognosis of Parkinson’s Disease?
Nicole: We're closer than we've ever been. One of the things that drove this work is the generation of patient cohorts and the participation of patients in research.
We have great models for Parkinson’s disease, but we need to understand what is going on with real-life, human patients. This is why The Michael J. Fox Foundation and other groups are investing in the development of patient cohorts and collecting a lot of information on the patients and their clinical symptoms.
We also monitor patients longitudinally, so that we can observe disease progression and look for changes in biofluid samples to see if there is a correlation between various readouts, like neuroinflammation, and disease state.
We are putting a huge effort into profiling these patients by looking at differences in DNA, RNA, lipids, inflammatory signatures, and other variables to understand Parkinson’s disease, the progression of the disease, and disease heterogeneity. It's probably not one thing that is going tell us whether you have Parkinson's or not, it's going to be this molecular signature that either increases or decreases your risk.
Elnaz: The idea of a multiomic signature is something that has taken a while to be accepted, but I think we are now starting to see it as a standard and accepted approach to identifying biomarkers.
What everyone recognizes is that while, for example, protein biomarkers do a tremendous job of indicating the presence of certain conditions, they might not be able to indicate the staging of a particular disease, or the degree of advancement, or the severity, and so on. Combining things like lipids or genomic markers will hopefully also reduce the likelihood of misdiagnosis.
What does the next year look like for PD research?
Nicole: Getting this profiling information from some of our cohorts is going be highly informative, particularly from the patients we’re tracking longitudinally. Looking at the samples from these patients and seeing if there are any leads that we can then move forward with is going to be huge.
Where can readers find more information?
About Dr. Nicole Polinski
 Nicole earned a bachelor’s degree in biology from Kalamazoo College and a doctorate in neuroscience from Michigan State University. Her previous research focused on characterizing and improving gene therapy in the aged brain for use in age-related neurodegenerative diseases such as Parkinson's.
Nicole earned a bachelor’s degree in biology from Kalamazoo College and a doctorate in neuroscience from Michigan State University. Her previous research focused on characterizing and improving gene therapy in the aged brain for use in age-related neurodegenerative diseases such as Parkinson's.
In addition to her experience researching Parkinson's disease, Nicole also has advocated for investment in neuroscience and Parkinson's disease research on Capitol Hill with the Society for Neuroscience and MJFF’s Public Policy Program.
At MJFF, Nicole manages the Preclinical Tools and Preclinical Models portfolios where she works with academic groups, contract research organizations, and pharmaceutical partners to facilitate the Foundation's efforts to generate, characterize, and widely distribute novel, research-enabling tools for the Parkinson’s drug development and fundamental research communities.
About Dr. Elnaz Atabakhsh
 Elnaz earned an Honors B.Sc. in Biochemistry from the University of Ottawa, and a Ph.D. in Biochemistry from The University of Western Ontario. She then went onto a post-doctoral fellowship at the Massachusetts General Hospital Cancer Center, prior to joining Abcam.
Elnaz earned an Honors B.Sc. in Biochemistry from the University of Ottawa, and a Ph.D. in Biochemistry from The University of Western Ontario. She then went onto a post-doctoral fellowship at the Massachusetts General Hospital Cancer Center, prior to joining Abcam.
Her research has focused on deregulation of signaling programs in cancer development and progression, as well as the mechanisms by which epigenetic modulators promote copy number variation in cancer.
In her current role as Senior Product Manager for Multiplex Assays at Abcam, Elnaz is responsible for shaping the vision for product development, commercialization, and collaboration projects related to the multiplex assays portfolio.