In a bid to understand the disease process caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), investigators have been trying to understand how the virus causes severe injury and sometimes death in a large percentage of cases. The researchers examined 17 adults, of median age 72 years, of which 12 were males. The median duration from hospitalization to death was 13 days.
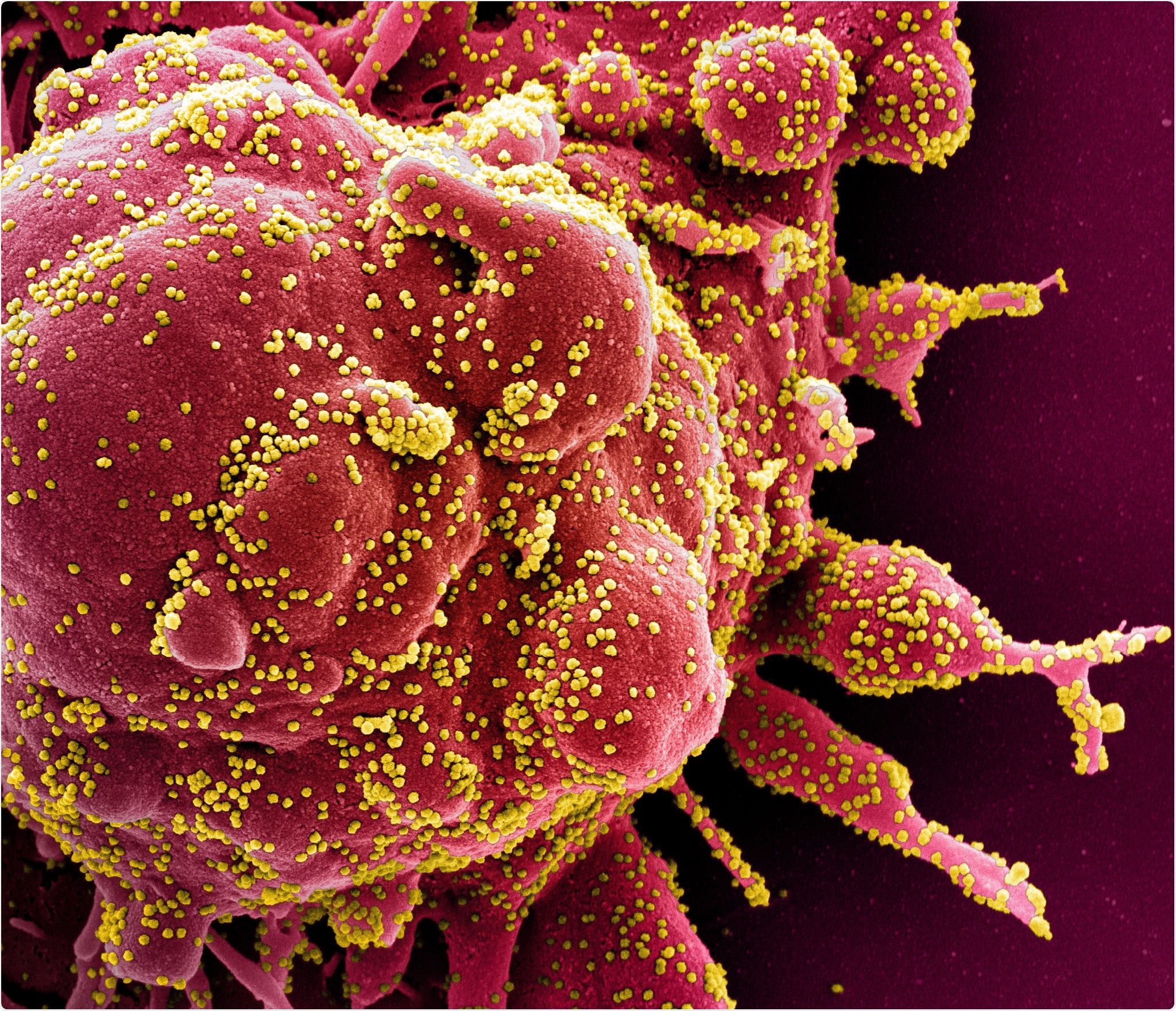
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of an apoptotic cell (red) heavily infected with SARS-COV-2 virus particles (yellow), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Except for 2 patients, all had one or more co-existing medical conditions, most commonly diabetes, and high blood pressure, at 9 and 10 patients, respectively. Another 4 each had cerebrovascular disease, coronary artery disease, and cancer.
Eleven and six patients died in the intensive care unit and the medical ward, respectively, with the chief causes of death being recorded as a respiratory failure in 9 cases and multiple organ failure in 7 cases.
What Did the Study Show?
Macroscopic examination of the lungs on autopsy showed a variety of findings, from heavy consolidated lungs to pulmonary artery thrombi. The heart was significantly larger than usual, and the liver in a few patients as well.
The kidneys were also larger in many patients, and looked pale but had no signs of blocked blood flow or hemorrhage. The gut was nonspecific, while the brain samples mostly showed no pathology.
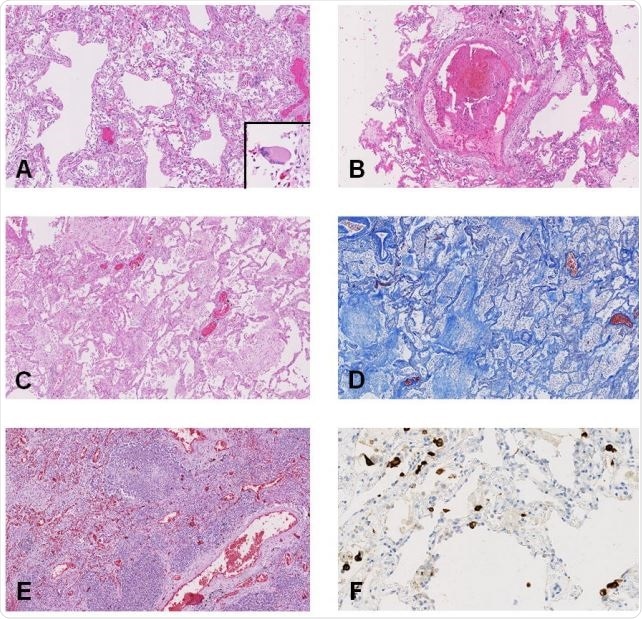
On histologic examination, the findings varied from diffuse alveolar damage (DAD) in the lungs, with microscopic clots within the small pulmonary arteries, acute pneumonic changes or bronchopneumonia, to chronic ischemic heart damage in a majority of patients, to congestive liver disease and fatty liver. The brain was hemorrhagic or suffused in about half the patients, but chronic changes were also frequently seen.
Of the 17 patients, 11 had the virus in their lungs when examined by immunohistochemistry, but in 16 by RT-PCR, which is more sensitive. The researchers failed to observe any uniform pattern of distribution of the virus in the lungs. At least one organ in every patient contained viral particles, mostly in the lungs, heart, liver, intestines, and a little less frequently in the spleen, kidney, and brain. The viral load was higher for tissues other than the lung.
Difficulties in Identifying a Specific Pattern of COVID-19 Injury
The aim of the study was to identify SARS-CoV-2-related organ injury. However, the autopsy results in these 17 patients showed signs of chronic disease overlaid by a variety of more recent signs. With gross differences in the co-morbidity pattern, treatment protocols, adoption of mechanical ventilation, and presence of acute complications, there is bound to be a diverse representation of lung injury.
For instance, in the case of DAD, it could have been part of the natural course of COVID-19 or alternatively, a result of other complications like hospital-acquired pneumonia. These are hard to differentiate in such critically ill patients, with over half of them showing acute pneumonic changes.
However, earlier researchers did conclude that COVID-19 pneumonia is not linked to DAD but to acute fibrinous and organizing pneumonia (AFOP). On the other hand, it is possible that AFOP could be a form of DAD that produces more fibrin.
The hyaline membranes characteristic of AFOP is also seen in DAD but with an unpredictable distribution. Thus, the whole lung must be examined to rule out the latter. Again, with lung biopsies, the presence of the virus could be missed in as many as half the cases. The study thus shows the potential error inherent in relying on lung biopsies and not whole lung studies to deduce the effects of this infection.
Pulmonary embolism was not very common, though microthrombi were seen frequently. Seven patients had either PE or pulmonary infarction; however, it was not the primary or major cause of death in this series of patients. Microthrombi are seen in many cases of Acute Respiratory Distress Syndrome (ARDS), and are a nonspecific feature of procoagulative and inflammatory states.
Acute cardiac injury was also not very common in the form of acute myocarditis or myocardial ischemia. The presence of the virus in all the tissues examined may reflect the widespread presence of the ACE2 receptor in the body and not direct viral injury.
Limitations and Implications
The study is limited in that only 17 patients were included, and the post-mortem examinations could be performed only 72-96 hours after death. This allowed significant autolysis to occur, leading to the destruction of tissues like the gut and kidneys. Another issue was the difficulty of tracing the timeline of viral spread between different organs, which might have helped to generate a theory as to the route of spread of the virus from the lungs to other parts of the body.
Finally, the course of the disease, the time to death, and the type of treatment was widely different, meaning that the findings could not be mapped to the microscopic findings as being results of COVID-19 itself, nor could the actual mechanism of organ injury be deciphered.
The absence of a specific pattern of injury in organs other than the lungs suggests that “SARS-CoV-2 infection may be just the trigger for an overwhelming host response, which could secondarily result in COVID-19-associated organ dysfunction.” Secondly, the detection of viral nucleic acid by the RT-PCR test need not mean the presence of actively replicating virus or even the presence of viral infection in the cell itself, but instead could be an innocuous finding.
The study, therefore, highlights the danger of mapping any single extrapulmonary feature of injury to COVID-19, while confirming the presence of the virus in every organ irrespective of whether lesions were seen on microscopic examination.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Remmelink, M., et al. (2020). Unspecific Post-Mortem Findings Despite Multiorgan 2 Viral Spread In COVID-19 Patients. medRxiv preprint. doi: https://doi.org/10.1101/2020.05.27.20114363. https://www.medrxiv.org/content/10.1101/2020.05.27.20114363v1
- Peer reviewed and published scientific report.
Remmelink, Myriam, Ricardo De Mendonça, Nicky D’Haene, Sarah De Clercq, Camille Verocq, Laetitia Lebrun, Philomène Lavis, et al. 2020. “Unspecific Post-Mortem Findings despite Multiorgan Viral Spread in COVID-19 Patients.” Critical Care 24 (1). https://doi.org/10.1186/s13054-020-03218-5. https://ccforum.biomedcentral.com/articles/10.1186/s13054-020-03218-5.