The COVID-19 disease pandemic caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has killed hundreds of thousands and infected millions around the world. While it presents with mild or asymptomatic infection in the majority of patients, it can lead to more severe manifestations, including often-fatal acute respiratory distress syndrome (ARDS) and multi-organ failure, in a significant minority of cases.
Many drugs and antivirals are being tested in hundreds of clinical trials around the world, including the lopinavir-ritonavir combination, hydroxychloroquine and azithromycin. However, the results so far have been disappointing, and the search for an effective treatment is still on.
What Are Interferons?
Interferons are natural chemicals that are secreted as part of the immune response to viral infections. They activate natural killer (NK) cells and macrophages, but SARS-CoV showed resistance to their effects by STAT1 inhibition that blocked IFN signaling.
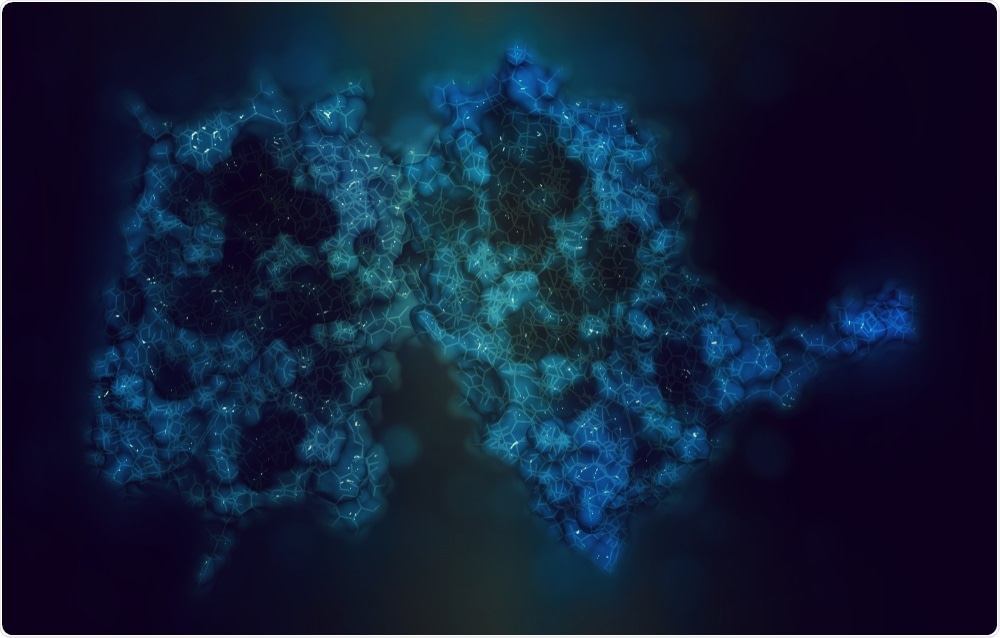
Interferon beta protein, Image Credit: StudioMolekuul / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The potential for the use of interferons in coronavirus infections was examined in the earlier outbreaks of SARS and MERS. In vitro experiments showed that interferons did have antiviral activity on the SARS-CoV, especially IFN-β and IFN-γ, and for IFN- β, against MERS-CoV as well.
Follow-up animal experiments showed that IFN-β had higher antiviral activity against MERS CoV compared to the lopinavir-ritonavir combination. The mechanism of action is via the interferon-stimulated gene (ISG), which arrests or delays viral replication. In addition, IFN β-1a reduces the incidence of complications following ARDS by improving vascular leakage, in addition to the antiviral activity. Thirdly, it increases the expression of the CD-73 protein, which could improve the outlook in patients.
These results failed to be replicated in more significant trials, though this could be due to the concomitant use of glucocorticoids, which are powerfully antagonistic to inflammatory responses. As of now, there are no published studies on the use of IFN β-1a in severe COVID-19. The current trial is aimed at establishing its clinical efficacy and safety in this situation.
Who Was Tested for IFN Therapy, and How?
The researchers designed an open-label randomized trial in adults aged 18 years or more, and who tested positive for COVID-19, or had clinical features strongly supporting this diagnosis. All participants were admitted to one Tehran, Iran, hospital between February 29 and April 3, 2020.
Severe COVID-10 was diagnosed by specific criteria, including hypoxemia, hypotension, renal failure, neurologic disorder, a low platelet count, severe digestive tract symptoms, all in relation to COVID-19, and with specific cut-off points.
The patients were randomly allocated to receive either standard of care or standard of care plus IFN β-1a. The dosage schedule was 44 micrograms/ml (12 million IU/ml) of interferon β-1a subcutaneously injected three times weekly for two consecutive weeks. Standard of care in this hospital comprised hydroxychloroquine (400 mg BD on the first day with 200 mg BD subsequently) plus lopinavir/ritonavir (400/100 mg BD) or atazanavir/ritonavir (300/100 mg daily) for 7-10 days.
Other drugs and therapies like deep vein thrombosis prophylaxis, azithromycin, other antibiotics, and steroids or intravenous immunoglobulins (IVIg) were given on a case-by-case basis. Overall, about 62% and 44% of patients in the IFN and control groups received steroids and IVIg in about 36% and 26%, respectively.
Demographic, baseline, and laboratory data were collected. The APACHE II score was calculated when any patient required admission to the intensive care unit (ICU).
The patients were followed up for four weeks. Regular assessment to fit in the 6-category ordinal scale was carried out on days 0, 7, 14, and 28. This includes discharge, hospital admission in 4 categories (without the need for oxygen, requiring oxygen, requiring non-invasive positive pressure ventilation (PPV), and requiring invasive mechanical ventilation), and death.
Following discharge, follow-up was conducted via telephone interviews. The records were surveyed for readmissions until May 3, 2020.
The researchers primarily assessed the time to clinical response, according to the ordinal scale mentioned above. Clinical response meant moving up two or more scores in the scale or being discharged from hospital, whichever came first.
Other outcomes included the duration of mechanical ventilation, hospital stay length, ICU stay length, the death rate at 28 days, and the effect of IFN therapy given early or late in the course of the disease, defined as before or after ten days of onset of symptoms.
The possible adverse effects of the two treatment protocols were also compiled, including allergic reactions, organ-specific injury, infectious complications, thromboembolic events, and septic shock.
More Discharges, Fewer Deaths with IFN
The study showed that of the 81 patients who took part in the study, 55% were men, aged 56 and 60 years on average, in the interferon and control groups, respectively. There were 42 and 39 patients in the two groups, respectively.
The most common coexisting illnesses at the time of admission were hypertension in about 40%, cardiovascular disease in about 30%, diabetes in 27%, along with high serum lipids, thyroid disease, and cancers (11% to 15%). The vital signs of patients in both groups were similar, but mean blood urea levels were more than twice as high in the IFN than the control group.
The primary outcome in both groups was comparable, with 9.7 vs. 8.3 days to clinical response in the IFN vs. standard of care groups. The number of discharges was more significant in the IFN group by day 14, at 68% vs. 44%. Early use of IFN was linked to lower mortality, with the odds nearly 14-times lower for death in the former case as compared to the latter.
The mortality at 28 days was also lower in the IFN group at 19% vs. 44%. Other complications were comparable. The IFN caused fever, chills, and myalgia in a fifth of patients, and one patient had an allergic reaction. Neuropsychiatric disturbances occurred in four patients, but only one was thought to be the result of IFN administration.
The present study thus shows that there is an increase in the number of patients discharged by day 14, the mortality rate by day 28, and a more significant benefit to early initiation of IFN therapy. While there were some side-effects, IFN was well tolerated.
The Implications: IFNs Could Help Treat COVID-19
Different types of IFN are being evaluated for efficacy in the current pandemic, such as IFN β-1b in combination with lopinavir-ritonavir and ribavirin in mild to moderate COVID-19, and nebulized IFN α-2b with oral arbidol.
The Iranian research study suggests that IFN β-1a added to the standard of care increased the proportion of patients discharged by day 14, and reduced the mortality at 28 days. Early administration of the drug improved survival rates. The tolerability and safety profile of the drug was also acceptable.
The study thus points to the need to confirm these findings and hopefully develop a more effective therapy for severe COVID-19 disease.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources