While earlier studies have shown the significance of serological testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in pregnant women, their partners have largely been excluded. Now, a new Danish study published on the preprint server medRxiv* in September 2020 reports the impact of serologic testing in both pregnant women and their partners, as well as their newborns.
The COVID-19 pandemic is transmitted mainly by droplets. However, several researchers have attempted to find out if vertical transmission occurs in pregnancy and parturition. Most such studies have focused on polymerase chain reaction (PCR) testing for viral RNA. One study found that of ~700 parturient women in New York City, the prevalence of COVID-19 was 10%, and ~80% were asymptomatically infected. The incidence of Cesarean sections, post-delivery issues, and placental disease appeared to be higher in infected mothers.
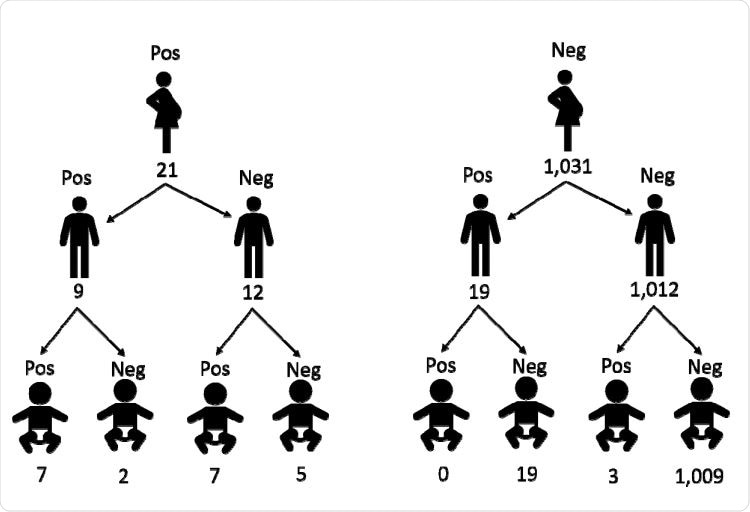
Serology in pregnant women has found a seroprevalence of about 6%. In the current prospective cohort study using broad serological testing, the researchers included over 1,300 women, ~1,200 partners, and 1,200 newborns, in over 1,000 families with complete serological data.
Pharyngeal swabs and blood samples were obtained on admission from all the women and their partners, and a blood sample from the umbilical cord immediately after parturition. All swabs underwent PCR for SARS-CoV-2 RNA, and serological assays were carried out on the blood samples.
Family pattern of SARS-CoV-2 transmission
Risk Higher by 37% in Women with Seropositive Partners
About 3% and 4% of mothers and their partners were seropositive, respectively, when corrected analyses are used. In families where the partner was seropositive, there was a 37% risk that the pregnant woman would be infected, which is almost half as much again compared to the risk faced by those living with seronegative partners. Seropositive women were more likely to have blood type A but had no significant differences from seronegative women.
The partners of these women also had no significantly different baseline characteristics except for comorbidities. About 60% reported COVID-19 symptoms. More seropositive men had a history of prior COVID-19-positive swabs and symptoms compared to seronegative men.
Overall, just over half of seropositive individuals were symptomatic.
Seropositivity in Newborns
Immunoglobulin G (IgG) antibodies against SARS-CoV-2 were present in 17 newborns, but no Immunoglobulin M (IgM). Of the seropositive newborns, three were born to seronegative mothers. Thus, the risk of seropositivity in the newborn was almost 450 times greater (or the baby was at 86% higher risk for antibody detection) if the mother was seropositive, compared to those born to seronegative mothers.
Of the 29 seropositive women, only one had a COVID-19 positive swab, while one in the seronegative group had a positive swab four days prior to delivery. The researchers found no apparent links between a past history of COVID-19 during pregnancy and complications to either the mother or newborn.
No Obstetric or Newborn Complications Detected
This study did not show any effect of the disease on the newborn in terms of weight difference, vigor or term of gestation. This contrasts with the New York City study mentioned above, where the rate of Cesarean delivery was ~46% in COVID-19 positive mothers but ~31% in uninfected women. The difference could be due to the criterial differences, where the current study relied on serology while the earlier one used PCR of nasopharyngeal swab specimens. Another possibility could be varying national guidelines for Cesarean section or variations in the baseline characteristics of the women in these two studies.
These differences can cause significantly varying study outcomes, as shown by the higher frequency of cesarean delivery (at 59% and 93%, respectively) in two different recent studies in women with symptomatic COVID-19 women.
The IgG antibodies in the newborns may be due to passive diffusion of antibodies across the placenta, unlike IgM. Thus they are not a reflection of vertical transmission but of maternal infection. The presence of antibodies in some seronegative mothers might be because of the concentration of maternal antibodies within the newborn’s circulation.
Another reason to rule out infant infection is the lack of adverse neonatal outcomes, without any indication of hypoxia, acidosis, malformations, or neonatal hospitalization.
Implications
Parturients are, in general, hospitalized only around childbirth, and thus represent typical women of their age in the community. Their partners also offer a window for assessing community prevalence of this virus. In the Danish population, the prevalence was estimated at 1% based on a sampling of 40% of the random population sample. The higher prevalence in this study could be due to the different timelines of these two estimates.
Overall, Denmark has reported low rates of infection due to an early lockdown. Still, women living with an infected partner have a higher risk of being infected themselves, even with the high rate of asymptomatic infection. Such studies are essential to understand how infection can spread within families and thus guide public health advisories and policies.
The study concludes, “This study reports no association between COVID-19 and obstetric or neonatal complications.” On the other hand, the risk of infection in women is increased when living with a seropositive partner.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Egerup, P. et al. (2020). Impact of SARS-CoV-2 Antibodies at Delivery in Women, Partners and Newborns. medRxiv preprint. doi: https://doi.org/10.1101/2020.09.14.20191106. https://www.medrxiv.org/content/10.1101/2020.09.14.20191106v1
- Peer reviewed and published scientific report.
Egerup, Pia, Line Fich Olsen, Ann-Marie Hellerung Christiansen, David Westergaard, Elin Rosenbek Severinsen, Kathrine Vauvert Römmelmayer Hviid, Astrid Marie Kolte, et al. 2020. “Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Antibodies at Delivery in Women, Partners, and Newborns.” Obstetrics & Gynecology 137 (1): 49–55. https://doi.org/10.1097/aog.0000000000004199. https://journals.lww.com/greenjournal/Abstract/2021/01000/Severe_Acute_Respiratory_Syndrome_Coronavirus_2.7.aspx.