How temperature affects the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been a question asked since the pandemic's early days. Just like the flu, which has a substantial seasonal variation, it is believed that SARS-CoV-2 also may be affected by temperature.
Some modeling studies indicate that cases will increase as the weather cools. Early studies using data from different countries looked at how fast the number of cases increased and suggested temperatures of 0–10 ºC were the most favorable for spread.
Models that incorporate weather data like humidity, temperature, pollution, and others do not generally have the statistical power to define how they affect the response accurately. Hence, when other inputs like demographics and time trends are added, their effect is lost. In addition, during the early stages of the pandemic, the quality of statistical data available may not have been very reliable.
Although current data reporting has become stable, there is still a difference between actual COVID-19 cases or deaths and when they are reported. Further adding the weather variables that could have influenced the event could add to the already present biological variations.
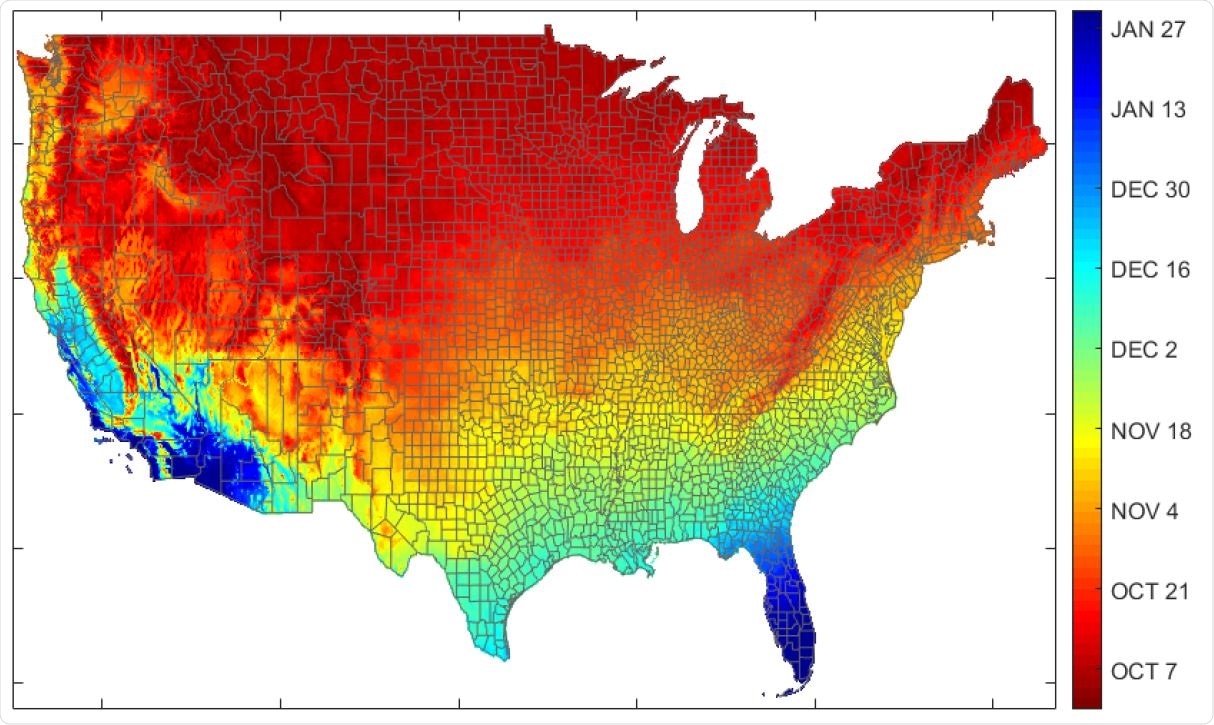
Expected date by U.S. county for entering 5-10°C range (30-year average).

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Modeling temperature response of COVID-19 cases
In a new modeling study published as a preprint paper on the medRxiv* server, a diverse team of researchers reports how SARS-CoV-2 transmission in the U.S. changes with temperature. The authors gathered about 2500 observations from April 16-July 15, 2020, on state-level deaths, positive cases, and tests. They obtained temperature data from the U. S. National Weather Service.
The researchers obtained weather data from airports with the most commercial traffic in each state. Because of this, measurement errors are small, write the authors, with about 60% of the U.S. population living within 300 km from the representative airport in their state.
Upon analyzing the data, they found that daily deaths fell from April to the end of May, and then became almost flat. At the same time, the temperatures were rising. As the temperature decreases to 10–5 ºC, there is an almost exponential increase in the number of positive cases.
Next, they simulated different scenarios for daily deaths from COVID-19 by changing the different variables they used in their model. Taking the data from Georgia as an example and changing the temperature from 31 ºC to 5 ºC, they found that daily deaths increased with decreasing temperatures.
It has been suggested that states like Hawaii that are geographically isolated and have small populations might have reduced COVID-19 deaths with warmer weather. However, the authors suggest this is unlikely, given previous reports that have suggested that increasing temperatures by itself is not enough to stop the spread of the virus.
The team also modeled the number of new positive cases as a function of temperature normalized to a value at 31 ºC. This is a temperature close to the summer maximums in the U.S. The model predicts that the number of new positive cases increases as the temperature decreases by almost 400% as temperature drops from 31 ºC to 5 ºC.
Cases projected to increase in winter
The model shows that the relationship between new positive cases and temperatures is more pronounced than the relationship between the deaths and temperature. Thus, although summer temperatures may be helping reduce virus transmission, transmission still needs to be brought under control.
Reducing temperatures with the advent of fall and winter will dramatically increase the number of positive cases and deaths, predicts the model.
Apart from a static model, the authors also developed a dynamic model where the temperature affected the daily deaths, and which is then used for further projections. Apart from the direct effect of temperature on the death counts, there is also an indirect effect, compounding the effect of temperature-driven daily deaths when the initial death counts lag this output in the simulation.
This dynamic model suggests a delay in responding to increasing positive cases with cooler temperatures will rapidly increase in cases. "This is already being seen in the current spatial pattern of outbreaks," write the authors.
Furthermore, according to the authors, summer's warmer temperatures may have helped reduce the number of cases and contributed to a false sense of the effect of the efforts. The winter will present more challenges with colder temperatures. Along with the fear of increasing flu during the winter months, COVID-19 transmission will also increase during these months.
The authors write, "Investment in providing the pandemic modeling community with timely counts based on death certificate dates would allow them to deliver substantially more accurate and timely warnings of impending upturns."

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources