The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of the ongoing COVID-19 pandemic, has resulted in significant morbidity and mortality – especially within the United States (US).
Accordingly, state-level re-openings that happened in spring 2020 created a perfect opportunity for the resurgence of SARS-CoV-2 transmission. During this period, one pertinent question was whether human contact and mixing patterns could increase gradually without the increase in viral transmission.
The rationale for the latter was that mixing patterns would likely be linked to better distancing, masking and hygiene practices. Moreover, there was also a question of whether the outbreak's clinical characteristics would improve after the inceptive surge of cases.
A group of researchers, led by Dr. Nathan Wikle from the Pennsylvania State University, analyzed the age-structured case, hospitalization, and death time series from the three US states (Rhode Island, Massachusetts and Pennsylvania) which have not experienced substantial epidemic rebounds during summer 2020 in comparison to March/April levels.
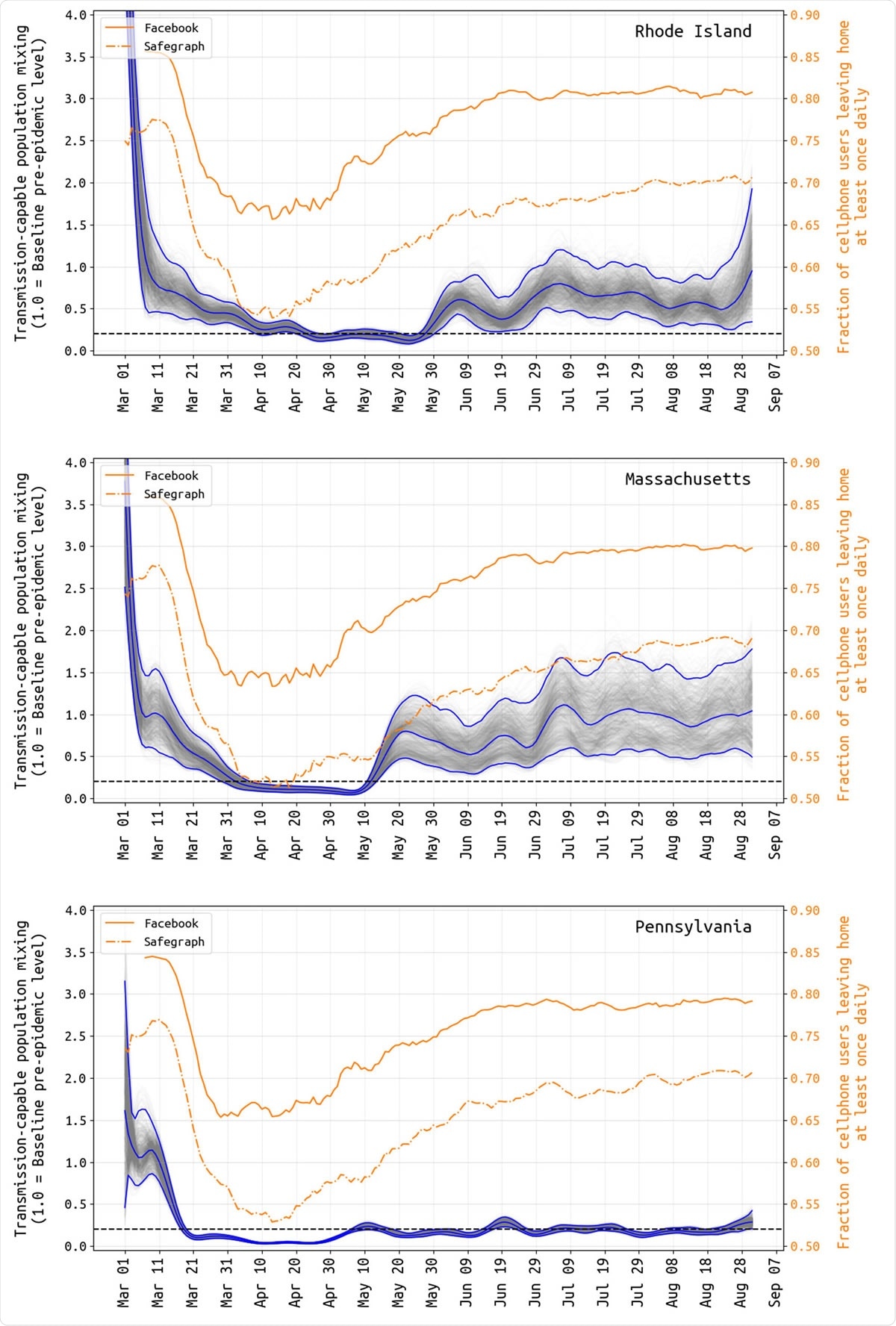
Transmission-capable mixing βt (in gray and blue) and mobility changes (yellow) from March 1 to August 31. The average population mixing for March 5-15 is set to 1.0 as the pre-epidemic level of transmission-capable mixing, and all other values are reported relative to this. Gray lines show 1000 sampled posterior β-trajectories with the blue lines showing the median and 95% credible intervals. Note that there is substantial uncertainty in these estimates during the first weeks of March, as case numbers were low and reporting may not have been catching a large proportion of true cases at this time. Yellow lines show the fraction of Facebook and SafeGraph users that left home at least once per day. The correlation between populationmovement (yellow) and transmission-capable population movement (gray+blue) begins to disappear in early May in all three states.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Evaluating epidemiological patterns and clinical data streams
These researchers evaluated eleven clinical data streams outlined by the respective state health departments in a Bayesian inference framework. Basically, this is constructed on an ordinary differential equation (ODE) age-structured epidemic model that entails compartments (i.e., clinical states) for hospitalization, critical care, and mechanical ventilation.
More specifically, they have inferred parameters on clinical characteristics, surveillance and transmission patterns of the first epidemic wave that took place in Rhode Island, Massachusetts, and Pennsylvania.
Then they have delineated the patterns of constantly low transmission in the three states mentioned above through August 31, subsequently comparing them to changes in human mobility metrics and appraising changes in age structure and clinical outcomes.
Finally, they have gauged the impact of the spring epidemic on elderly populations in these three states and compared infection fatality rates to the available estimates from other parts of the US.
Shifts in age structure and clinical outcomes
"We show that population-average mixing rates dropped by more than 50% during the lockdown period in March/April and that the correlation between overall population mobility and transmission-capable mobility was broken in May as these states partially reopened", say study authors in this medRxiv paper.
In their analysis, infection fatality rates were estimated to be higher when compared to the recently published summary studies, with the differences particularly notable in the 60-79 age group where the rates were 1.5 to 2.5 times as high.
Likewise, the researchers have demonstrated that elderly individuals were much less able to decrease contacts during the lockdown period than younger individuals, leading to the outbreak concentrating within elderly congregate settings – despite the lockdown.
Furthermore, the study has also suggested that individuals infected during the spring wave and summer interval were more likely to progress to symptomatic disease in comparison to the average person in the population.
This is actually consistent with the observation that children were the least exposed during the spring and summer months. Hence the exposed population was more prone to progress to apparent symptoms and more likely to develop severe clinical outcomes.
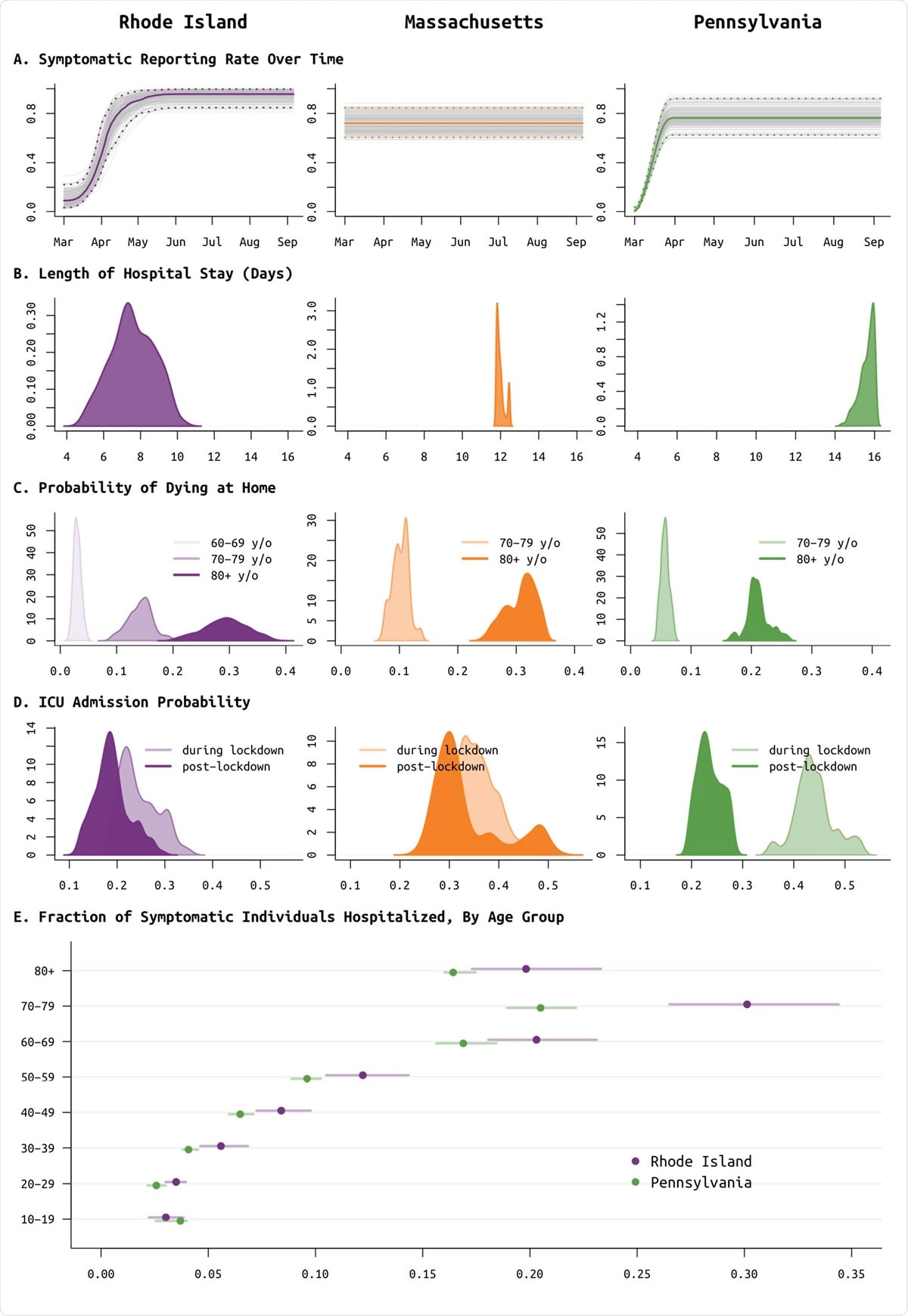
Posterior distributions of reporting rate (panel A) and clinical parameters (panels B to E) for Rhode Island (purple, left column), Massachusetts (orange, middle column), and Pennsylvania (green, right column). (A) Reporting parameter ρ, i.e. the fraction of symptomatic SARS-CoV-2 cases that are reported to the health system, plotted as a function of time. In Rhode Island, it was known that in March testing was not available and cases could not be confirmed; therefore a spline function was fit for ρ. This same function provided a better fit for Pennsylvania data, but not for Massachusetts data. (B) Median length of medicalfloor hospital stay was 7.5 days in RI, 11.9 days in MA, and 15.7 days in PA. This parameter was constrained to be between 11.8 and 12.8 days in MA, as without this constraint identifiability issues arose due to the lack of the ‘cumulative hospitalizations’ data stream. (C) Probabilities of dying at home for the 60-69, 70-79, and 80+ age groups; 60-69 age group was included only for RI as data were insufficient in PA and MA. These are largely reflective of the epidemics passing through nursing home populations where individuals are not counted as hospitalized if they remain in care at their congregate care facility in a severe or advanced clinical state. These probabilities are important when accounting for hospital bed capacity in forecasts. (D) Age-adjusted ICU admission probability during the lockdown period in spring 2020 (lighter color) and after the lockdown (darker color). (E) Probability of hospitalization (median and 95% CIs) for symptomatic SARS-CoV-2 infections, by age group; MA estimates are excluded as these had priors set based on estimates in RI.
How to protect the most vulnerable?
In a nutshell, statistical inference described in this paper on attack rates, underreporting and shifting age-profiles may actually provide improved guidance for real-time decision making and adequate public health messaging.
"As recent policy discussions have been diverted by the capitulation and laziness of an epidemic management approach that would encourage younger/healthier populations to become infected, we should restate that our state-level analyses indicate that older individuals are not able to fully isolate during lockdown periods", accentuate study authors.
Basically, this means that 'protecting the vulnerable' strategy is unworkable, as more endangered individuals will still necessitate essential care and contact. Thus, any policy aiming to protect just the vulnerable while granting the rest of the population to move freely would almost certainly fail at preventing viral introduction.
In conclusion, as individuals in the oldest age groups are more or less unaffected by the lockdown, the best solution to protect these (but also other) vulnerable populations is to limit the spread in the general population.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Wikle, N. et al. (2020). SARS-CoV-2 epidemic after social and economic reopening in three US states reveals shifts in age structure and clinical characteristics. medRxiv. https://doi.org/10.1101/2020.11.17.20232918, https://www.medrxiv.org/content/10.1101/2020.11.17.20232918v1
- Peer reviewed and published scientific report.
Wikle, Nathan B., Thu Nguyen-Anh Tran, Bethany Gentilesco, Scott M. Leighow, Emmy Albert, Emily R. Strong, Karel Brinda, et al. 2022. “SARS-CoV-2 Epidemic after Social and Economic Reopening in Three U.S. States Reveals Shifts in Age Structure and Clinical Characteristics.” Science Advances 8 (4). https://doi.org/10.1126/sciadv.abf9868. https://www.science.org/doi/10.1126/sciadv.abf9868.