In the search for effective antivirals to prevent and treat severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, scientists have investigated the possibility of inhibiting the main viral protease (Mpro), and papain-like protease (PLpro), that are key to its replication. Many compounds that inhibit these enzymes have been described and are advancing through the drug development pathway.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
These two proteases are cysteine proteases, encoded as nonstructural protein (nsp) 3 and nsp 5. Of these, Mpro is autocleaved from a large polyprotein and then dimerize to form the mature functional protein. They are required to cleave the large viral polyprotein into its several functional parts in order for them to help set up the transcription-replication complex near the sites of virus assembly within the infected host cells. If one or both are inhibited, viral RNA is suppressed and infection cannot be established.
Many Mpro inhibitors have been identified, including covalent compounds with electrophilic warheads, and one has entered clinical trials in humans. The same is not true of the PLpro because it preferentially attaches large ubiquitin-like protein substrates. Thus, the best PLpro inhibitors seem to be those that bind to the non-enzymatic sites that recognize ubiquitin.
Issues with Mpro/PLpro inhibitors
Earlier protease inhibitors targeting other RNA viruses have been difficult to develop, and this could predict similar obstacles in the path of the current attempt. For one, the initial autocleavage of Mpro is not easily prevented, given the favorable energy profile of the intramolecular reaction.
Secondly, the dimeric Mpro is aggregated at specific locations in the cytosol or at the membrane surfaces near the viral polyprotein. Thus, the substrate levels are quite high in the enzyme's proximity, making competitive inhibition unlikely.
Thirdly, many viral proteases tend to keep their cleavage products bound within the substrate cleavage sites. This means they are slow to bind to the inhibitor unless the cleaved substrate is first displaced – termed product inhibition. And Mpro has an active site where an inhibitor can act only after its monomer is formed, making it impossible to prevent this step.
In short, the scientists point out, the only possible inhibitors are those which are highly bioavailable, and can reach local concentrations high enough to competitively inhibit the original substrates, and thus achieve early inhibition before active replication begins.
Cross-reactivity of protease inhibitors
Again, protease inhibitors tend to bind to any host protease with a similar preferred substrate range. Redundancy of enzyme pathways in the host cell is another challenge. A range of cell systems is used to study these lead inhibitors, which means they express various proteases over different levels.
For instance, many proteases can accomplish cleavage of the S protein of SARS-CoV-2 to facilitate viral fusion, including cysteine cathepsins B and L, and TMPRSS2. All of these are present at high levels on lung cells, but their expression on experimental cell lines varies. This means nobody quite knows for sure which cell type is actually the most accurate reflection of the primary infection site in a living host, and that it may not be possible to target any of them singly since the others provide an escape pathway.
Mpro inhibitors disarmed by TMPRSS2 expression
In the current study, the researchers selected six electrophilic warhead-bearing covalent compounds that inhibited recombinant Mpro in a time-dependent fashion, out of around 650 molecules that target cysteine residues in Mpro and PLpro. They were unable to find any leads for PLpro inhibitor development, perhaps because of the very narrow range of suitable substrates.
Two of the six appeared to have antiviral activity by Mpro inhibition in the modified lung adenocarcinoma cell line A549. There is a significant difference in the potency in cellular infection assays compared to in vitro tests, because of the effect of cellular uptake and the need to completely inhibit Mpro within the host cell.
However, when tested in cells expressing TMPRSS2, their observed potency dropped sharply. The virus achieved entry into the host cell via TMPRSS2, indicating that the supposed Mpro inhibitor actually only succeeded in inhibiting cathepsin. This activity was further confirmed.
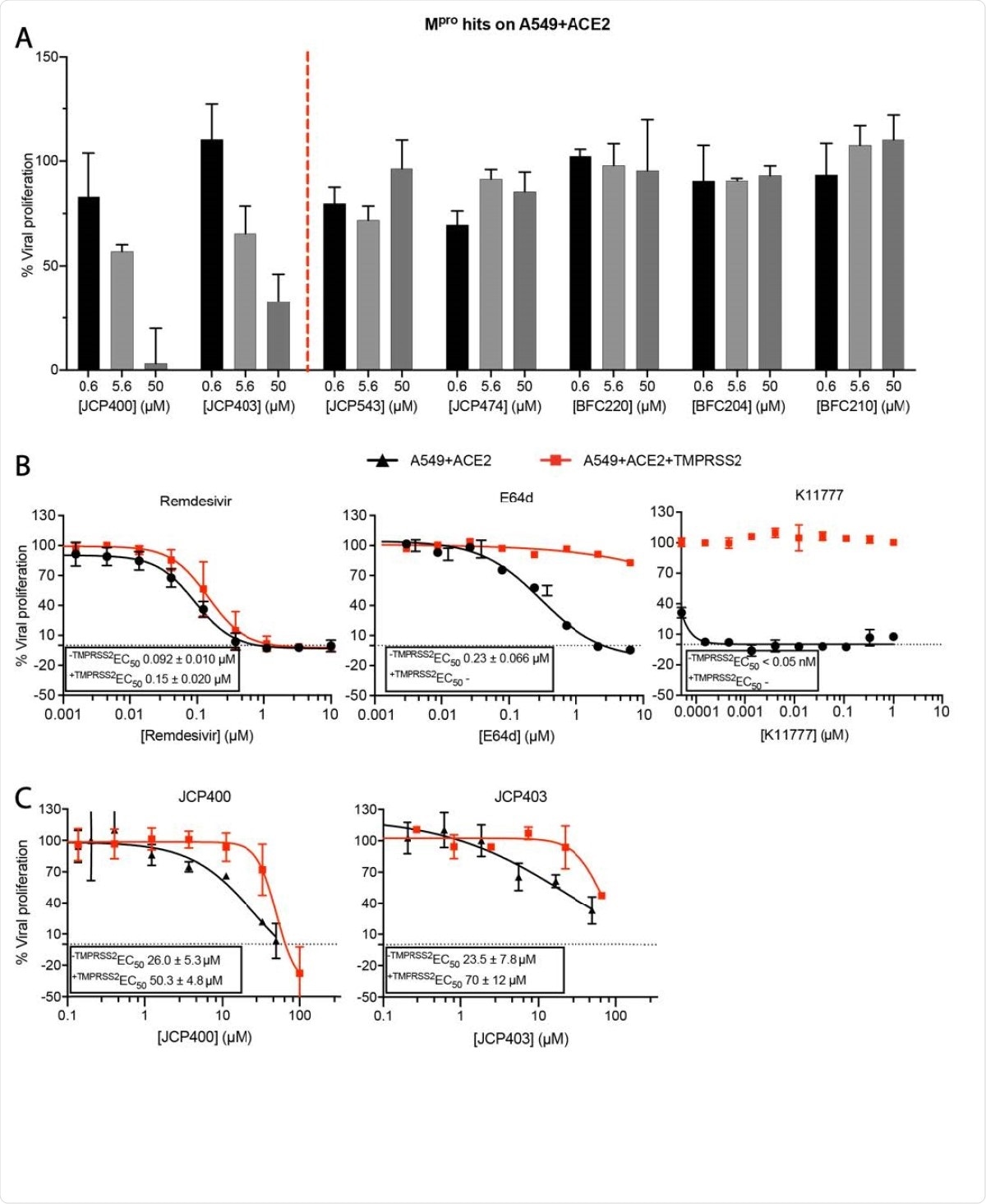
Potency of Mpro hits in cellular SARS-CoV-2 infection assays. A) Two out of six newly identified Mpro inhibitors are active in A549+ACE2 infection model. B) SARS-CoV-2 inhibition curves of Remdesivir, E64d and K11777 in A549+ACE2 cells with or without expression of TMPRSS2. C) SARS-CoV-2 inhibition curves of Mpro inhibitors JCP400 and JCP403 in A549+ACE2 cells with or without expression of TMPRSS2. Data are means ± SD of two replicate experiments.
Thus, these lead compounds resemble known cysteine cathepsin inhibitors and many Mpro inhibitors were reported earlier, which were also found to be inhibitors of the cathepsins at nanomolar concentrations.
What are the implications?
The researchers emphasize that though many potential Mpro and PLpro inhibitors are being explored for the treatment of SARS-CoV-2 infection, it is important to ensure that these compounds are indeed selective for these enzyme targets, rather than inhibitory for other redundant cellular pathways. For instance, rupintrivir, a supposed Mpro inhibitor, is a highly potent cathepsin L inhibitor, and this accounts for the observed antiviral activity.
Secondly, inhibition of viral replication is not a proxy for selective target enzyme inhibition, since the former can occur through other pathways as well. The latter must be directly confirmed before a lead molecule can be said to have the desired efficacy. The ability to inhibit the catalysis of a substrate of Mpro, or to label the active Mpro enzyme, is a very recent metric to evaluate Mpro activity within a cell, in fact.
Thirdly, cell lines must be appropriately selected to test antiviral activity so as to enable the identification of inhibitors that act through redundant viral entry pathways.
The authors sum up, "We strongly believe that our findings are of particular importance in light of drugs that are widely suggested for advancement into clinical trials such as rupintrivir, or even have entered clinical trials such as K11777 and PF-07304814."

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Steuten, K. et al. (2020). Challenges for targeting SARS-CoV-2 proteases as a therapeutic strategy for COVID-19. bioRxiv preprint. doi: https://doi.org/10.1101/2020.11.21.392753,https://www.biorxiv.org/content/10.1101/2020.11.21.392753v1
- Peer reviewed and published scientific report.
Steuten, Kas, Heeyoung Kim, John C. Widen, Brett M. Babin, Ouma Onguka, Scott Lovell, Oguz Bolgi, et al. 2021. “Challenges for Targeting SARS-CoV-2 Proteases as a Therapeutic Strategy for COVID-19.” ACS Infectious Diseases 7 (6): 1457–68. https://doi.org/10.1021/acsinfecdis.0c00815. https://pubs.acs.org/doi/10.1021/acsinfecdis.0c00815.