The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection caused by coronavirus disease (COVID-19) induces hyperinflammatory and hypercoagulable states, leading to arterial and venous thromboembolic events. These conditions may cause severe complications and can be potentially fatal.
Now, researchers at Rutgers Robert Wood Johnson Medical School report the first case of COVID-19 triggering a rare occurrence of potentially severe blood clots forming in the arms.
The case report, published in the journal Viruses, sheds light on how hyperinflammatory states during COVID-19 can lead to upper extremity blood clots, called deep vein thrombosis (DVT).
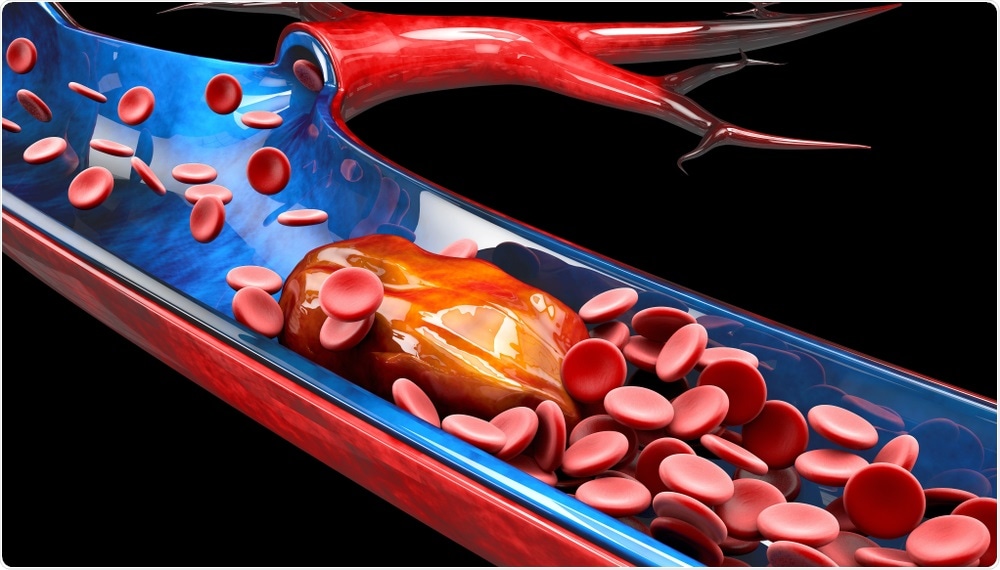
Deep Vein Thrombosis. Image Credit: Victor Josan/Shuttertso
What is deep vein thrombosis (DVT)?
Deep vein thrombosis (DVT) has been reported in COVID-19 patients. This is a serious condition that occurs when a blood clot forms in a vein located deep inside the body. Deep vein blood clots typically form in the thigh or lower leg, but can also develop in other body areas.
The most common signs and symptoms of DVT include cramping or throbbing pain in one leg, usually in the calf or thigh. It can also form in other parts of the body. Along with the cramps, the patient may experience swelling in one leg, warm skin around the tender area, red or darkened skin around the affected area, red or darkened skin around the area, and swollen veins.
High-risk individuals for DVT include those who are over 60 years old, overweight, those who smoke, have had DVT before, taking contraceptives or hormone replacement therapy, have cancer or heart failure, and those who have varicose veins.
Most DVTs occur in the lower extremities, called lower extremity DVT, due to the increased gravitational stress and reduced endothelial fibrinolytic activity compared to upper extremity veins. However, 4 to 10 percent of DVTs happen in the upper extremities, called upper extremity DVT (UEDVT).
Although rare, UEDVT can cause severe complications such as post-thrombotic syndrome, pulmonary embolism, and death.
Case report
In the study, the researchers described the case of an 81-year-old patient who had UEDVT in 2017. The male patient had a past medical history of high blood pressure, type 2 diabetes mellitus, coronary artery disease, heart attack or myocardial infarction with residual ischemic cardiomyopathy, and hypercholesterolemia.
The patient is a smoker, with 15 years of tobacco use but had a very active lifestyle, bicycling and playing tennis weekly until he developed cardiac symptoms.
In November 2016, he underwent a biventricular pacemaker upgrade. Due to this surgery, he was advised to refrain from upper extremity movement for six weeks. After, he resumed playing tennis.
While playing tennis, 42 days post-procedure, the patient had a left upper arm swelling from the top of the wrist to his shoulder lasting for four days. The patient presented to his primary care physician and was sent to the hospital for further management.
The patient received treatment and recovered. In February 2017, he underwent thrombectomy and angioplasty. He remained physically active and continued playing tennis three times a week.
In November 2020, the patient developed another left-arm swelling and sought medical attention. He noted the swelling for seven days, without pain, chest pain, or shortness of breath. He was admitted to the hospital for further management, but tested positive for SARS-CoV-2 as per hospital protocol to have patients tested.
There, he was diagnosed with an upper arm blood clot and was treated awaiting COVID-19 test results.
“Often, blood clots are preceded by chronic inflammatory conditions exacerbated by immobility, and rarely do they occur in patients who are otherwise healthy and active at baseline,” Payal Parikh, an assistant professor of medicine at Rutgers Robert Wood Johnson Medical School and study co-author, said in a statement.
After treatment, the patient was discharged the next day but had a positive test result for SARS-CoV-2 infection. He had asymptomatic COVID-19 and was advised to self-quarantine for 10 days. He was asymptomatic and his blood oxygen levels were not diminished.
Based on the case report, the researchers noted that an important area of COVID-19 research is finding the link between COVID-19 and thrombosis. The risk of thrombosis reflects the Virchow triad of endothelial injury, hypercoagulable state, and stasis.
In COVID-19, the virus can invade the endothelial cells through the angiotensin-converting enzyme 2 (ACE2) receptors, activating the renin-angiotensin system to increase angiotensin II levels. As a result, this promotes the expression of tissue factor and plasminogen activator inhibitor 1, promoting coagulation. Further, endothelial injury to the blood vessel is enhanced by the release of inflammatory cytokines.
The team also recommended that due to the increased thrombosis risk, COVID-19 patients should have tests like complete blood count (CBC), partial prothrombin time (PTT), activated partial prothrombin time (aPTT), D-dimer assays, and fibrinogen upon admission.
“During these pandemic times, we recommend considering SARS-CoV-2 infection as the etiology of venous thromboembolic events whether in the presence or absence of characteristic COVID-19 symptoms,” the team explained in the study.
“With insufficient knowledge of prophylactic strategies for UEDVT patients, further investigation is needed to determine optimal approaches for treating and preventing UEDVT recurrence during the COVID-19 pandemic and beyond,” they concluded.