Previous studies have already suggested that the time of day in which someone catches coronavirus disease 2019 (COVID-19) can play a critical role in the progression of this disease. This dynamic has also been reported with other viral pathogens, including parainfluenza type 3, respiratory syncytial, and influenza viruses.
Recently, scientists at the Aix-Marseille University in France have analyzed the implications of circadian rhythms (CRs) in the infection by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is the virus responsible for COVID-19, on isolated human monocytes, which are critical cells in COVID-19, in healthy individuals. The study, which was published in Microbial Pathogenesis, showed that the time of day of SARS-CoV-2 infection could impact the severity of the viral infection and the host immune response.
 Study: Daytime variation in SARS-CoV-2 infection and cytokine production. Image Credit: Quality Stock Arts / Shutterstock.com
Study: Daytime variation in SARS-CoV-2 infection and cytokine production. Image Credit: Quality Stock Arts / Shutterstock.com
Circadian rhythms and the immune system
The body’s CR regulates numerous physiological processes throughout the day. The rhythmic regulation of CRs is dependent upon both central and peripheral oscillators that are managed by BMAL1, which is the main clock gene.
In addition to regulating physiological processes each day, CRs also play a role in determining the individual’s susceptibility to certain viral infections. To this end, recent studies have shown that the time of day of an infection can be critical for the progression of disease with other viruses. The team thus aimed to determine the role of the CRs on COVID-19 progression.
“Clearly, the evidence of an implication of CR in SARS-CoV-2 infection of human cells are lacking… In this study, we wondered if SARS-CoV-2 infection and cytokine production by human monocytes, innate immune cells affected by COVID-19, were regulated by CR.”
The study
The researchers examined circadian oscillations of resting monocytes. Every three hours during the 24-hour cycle, total ribonucleic acid (RNA) was extracted, with the expression of BMAL1 and CLOCK genes studied in unstimulated monocytes.
The team also exposed monocytes to SARS-CoV-2 via One-Step real-time quantitative reverse transcription-polymerase chain reaction (qRT-PCR) and immunofluorescence. They also measured the interleukin (IL)-6, IL-1β, and IL-10 levels in the supernatants of infected monocytes.
COVID-19 can cause severe illness due to a cytokine storm, wherein high levels of proinflammatory cytokines, including the IL-6, IL-1β, and IL-10, are circulating in the body. The team aimed to determine the interaction of SARS-CoV-2 with monocyte-affected cytokine production at two time points over a 24-hour period.
Study findings
The BMAL1 and CLOCK transcripts were found to exhibit CRs in monocytes with an acrophase and a bathyphase at Circadian Time (CT)6 and CT17. CT6 and CT17 were chosen in this study as these two time points represent the beginning of both the active and resting periods in humans. After about 48 hours, the amount of SARS-CoV-2 was found to be significantly greater in infected monocytes at CT6 as compared to CT17.
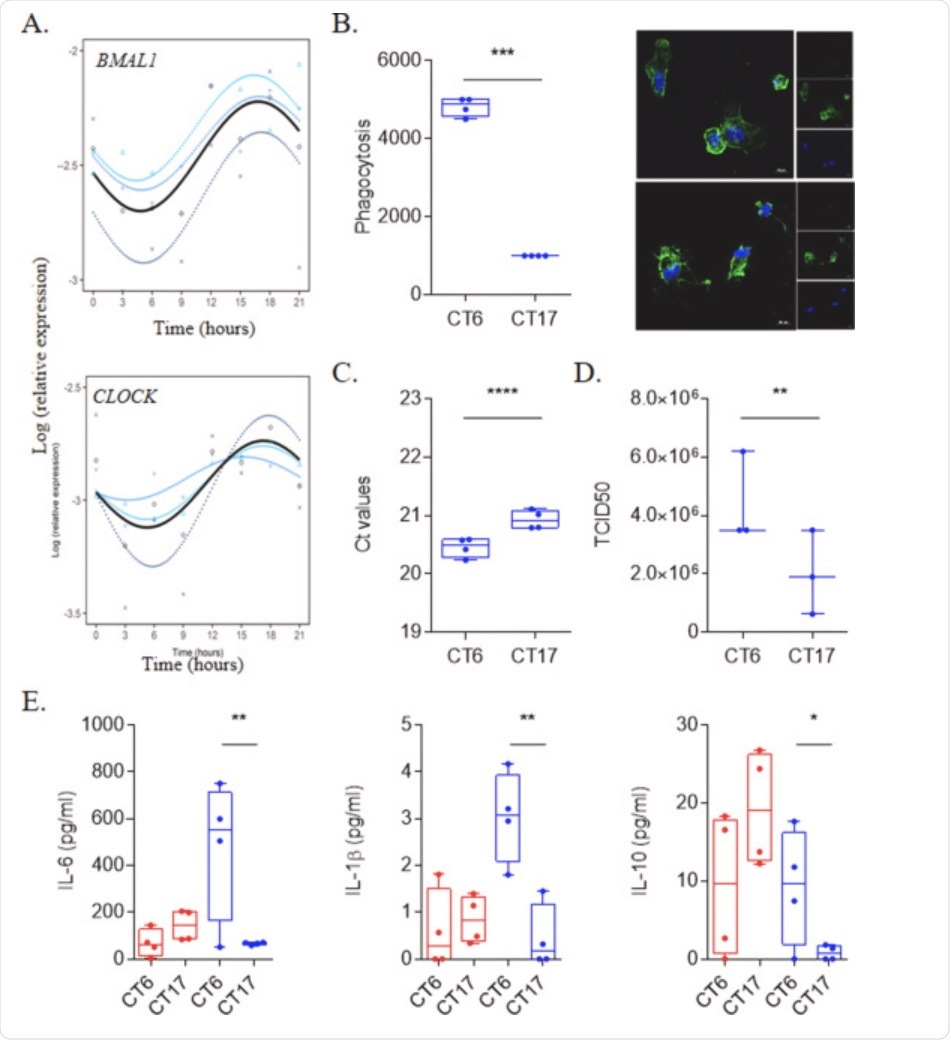 Fig. 1. SARS-CoV-2 infection is link to circadian rhythm. (A) Circadian rhythm of BMAL1 and CLOCK genes in monocytes using Cosinor model from 4 different donors. (B) Virus load (n = 4) and titers (n = 3) at CT6 and CT17 time from experiments that were repeated 3 times using at least 3 different donors. (C) Representative pictures and phagocytosis activity of monocytes (F-actin in green and nucleus in blue) infected by SARS-CoV-2 virus (red). Results are expressed as the mean ± SEM of 4 donors with 3 independent experiments. (D) Level of IL-6, IL-1β and IL-10 of unstimulated (red) and infected cells at CT6 and CT17. Results are expressed as the mean of 4 donors from 3 independent experiments.
Fig. 1. SARS-CoV-2 infection is link to circadian rhythm. (A) Circadian rhythm of BMAL1 and CLOCK genes in monocytes using Cosinor model from 4 different donors. (B) Virus load (n = 4) and titers (n = 3) at CT6 and CT17 time from experiments that were repeated 3 times using at least 3 different donors. (C) Representative pictures and phagocytosis activity of monocytes (F-actin in green and nucleus in blue) infected by SARS-CoV-2 virus (red). Results are expressed as the mean ± SEM of 4 donors with 3 independent experiments. (D) Level of IL-6, IL-1β and IL-10 of unstimulated (red) and infected cells at CT6 and CT17. Results are expressed as the mean of 4 donors from 3 independent experiments.
In addition to an increase in viral uptake by the monocytes, the researchers also found higher amounts of both SARS-CoV-2 RNA and titers to be higher in the supernatants of infected monocytes at CT6 as compared to those collected at CT17. This finding was significant, as it was the first time that the entry and multiplication of SARS-CoV-2 in monocytes were reported to change based on the time of day that the infection took place.
The researchers were also interested in determining whether the interaction of SARS-CoV-2 at CR6 and CR17 would also affect cytokine production at these two time points. To this end, the researchers found that IL-6, IL-1β, and IL-10, all of which are elevated during the COVID-19 cytokine storm, are significantly higher at CT6 as compared to CT17.
Since CT6 is also when SARS-CoV-2 infection appears to be at its highest, the researchers drew the conclusion that the interaction of SARS-CoV-2 with monocytes at this time also resulted in a distinct cytokine pattern that could be indicative of a cytokine storm.
Conclusion
“Our data showed for the first time that entry and multiplication of SARS-CoV-2 in human monocytes varies with the time of day. This finding is reminiscent of what has been previously reported with herpes and influenza virus in murine models of infection.”
Taken together, the findings discussed here suggest that SARS-CoV-2 likely manipulates the CR for its own gain. Therefore, CR represents a potential therapeutic target for healthcare providers in managing the progression of COVID-19.
This study also highlights that the timing of treatment administration to COVID-19 patients is crucial in preventing disease progression. These treatments include passive immunization, cytokines, anti-cytokine antibody or corticoids. All these drug candidates affect the immune response that may oscillate during the day and their administration according to the CR of SARS-CoV-2.