 By Neha MathurReviewed by Danielle Ellis, B.Sc.Nov 25 2021
By Neha MathurReviewed by Danielle Ellis, B.Sc.Nov 25 2021New Zealand has experienced one of the lowest mortality rates among all countries during the coronavirus disease 2019 (COVID-19) pandemic. To date, the country has reported 10,790 severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections and 41 deaths in total.
The country reported only 22 deaths from a total of 1,504 cases before successfully eliminating COVID-19 by June of 2020. In their endeavors to prevent a fatal outbreak, New Zealand implemented an alert level (AL) system that included stay-at-home orders and border restrictions. A delay in implementing these interventions would have drastically reduced their effectiveness and called for their continuance for an indefinite time.
Study design
A study published in the journal Royal Society Open Science demonstrates the critical role of timely intervention in New Zealand's success story. The researchers used a stochastic branching process model to simulate the trajectory of COVID-19 transmission and control during New Zealand's 2020 outbreak. They calculated the number of reported cases and deaths and the probability of elimination within a defined time frame.
 Study: Early intervention is the key to success in COVID-19 control. Image Credit: mustafaclk / Shutterstock
Study: Early intervention is the key to success in COVID-19 control. Image Credit: mustafaclk / Shutterstock
Three classes of interventions chosen for the study were as follows: (i) self-isolation/home quarantine, (ii) government-managed isolation (MIQ) and quarantine, (iii) population-wide control. Only MIQ was assumed to be 100% effective in preventing onward transmission. Due to restrictions under each of the four ALs, the population-wide control intervention simulated a reduction in transmission rate by a factor C (t) at time t. While the relative transmission rate C (t) was equal to one in the absence of population-wide control, it had smaller values at higher ALs. Besides, higher ALs also resulted in a reduction in effective reproduction number (Reff). Note that Reff impacts the probability of extinction in a branching process and is related to the rate of exponential growth during the early phase of an outbreak.
The researchers explored seven scenarios during the study - scenarios 0, 1, 2, 3, 4, 5, and 6. The duration of each AL was the same in each scenario – 33 days at AL4 followed by 16 days at AL3.
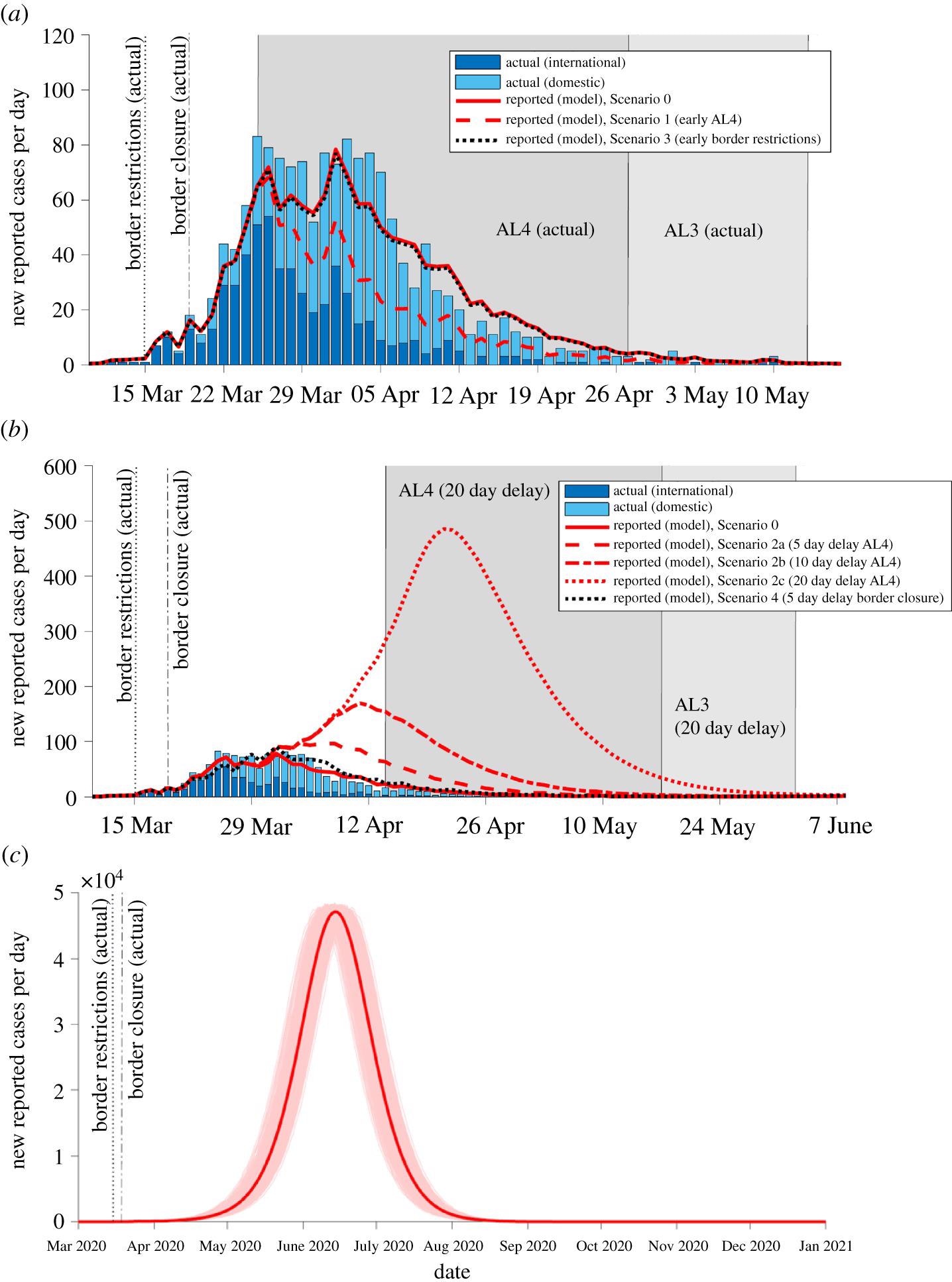 Effect of alternative timings of interventions on the trajectory of the outbreak. Number of new reported cases per day predicted by the model (averaged over 5000 simulations) alongside observed reported domestic (light blue bars) and international cases (dark blue bars) (data source: MoH). Model simulated for interventions implemented on their actual start dates and for alternative scenarios with different timings of AL4, border restrictions or border closure (a) Scenario with AL4 started 5 days early (border restrictions and closure on actual start dates) (red dashed; Scenario 1) compared with a scenario where border restrictions were implemented five days early (border closure on actual start date) (black dotted; Scenario 3). (b) Delayed start to AL4 (delays of 5, 10 and 20 days; Scenarios 2a–c; red broken lines) (with border restrictions and closure on actual start dates). Five-day delay to border closure (with border restrictions and AL4 on actual start dates) (black dotted; Scenario 4). (c) No AL4/3 restrictions (border restrictions and closure on actual start dates; Scenario 6) results in an uncontrolled outbreak; faint red lines show the outbreak in individual realizations of the model, the bold red line is the average over all 5000 simulations. Note, x- and y-axis scale differs between figures.
Effect of alternative timings of interventions on the trajectory of the outbreak. Number of new reported cases per day predicted by the model (averaged over 5000 simulations) alongside observed reported domestic (light blue bars) and international cases (dark blue bars) (data source: MoH). Model simulated for interventions implemented on their actual start dates and for alternative scenarios with different timings of AL4, border restrictions or border closure (a) Scenario with AL4 started 5 days early (border restrictions and closure on actual start dates) (red dashed; Scenario 1) compared with a scenario where border restrictions were implemented five days early (border closure on actual start date) (black dotted; Scenario 3). (b) Delayed start to AL4 (delays of 5, 10 and 20 days; Scenarios 2a–c; red broken lines) (with border restrictions and closure on actual start dates). Five-day delay to border closure (with border restrictions and AL4 on actual start dates) (black dotted; Scenario 4). (c) No AL4/3 restrictions (border restrictions and closure on actual start dates; Scenario 6) results in an uncontrolled outbreak; faint red lines show the outbreak in individual realizations of the model, the bold red line is the average over all 5000 simulations. Note, x- and y-axis scale differs between figures.
Key findings in each scenario
In scenario 0, border closure and AL4 were implemented on the dates they actually occurred. In this scenario, the expected values of the key measures were the same as the observed values. In the AL4, the expected and the actual number of daily reported cases leveled off at 70–80 for around one week before declining again.
In scenario 1, wherein AL4 was implemented 5 days earlier, the actual values of most of the key measures were slightly lower than the observed values. The daily new cases peaked at 69 around 26 March and dropped again at the end of AL4. The findings from this scenario suggest that an infected individual is most infectious during AL3, where Reff is higher and infects more people, on average, in this scenario than in scenario 0.
In scenario 2, where AL4 was delayed by 20 days, a higher peak in daily new cases and greater cumulative totals of cases and deaths were observed. In scenario 3, while border restrictions were imposed five days earlier, border closure and AL4 started on actual dates, which had little impact on the initial trajectory or eventual outbreak size. The values of all the key measures remained the same as in scenario 0 as they are more sensitive to variations in the timing of AL4 than the timing of border restrictions.
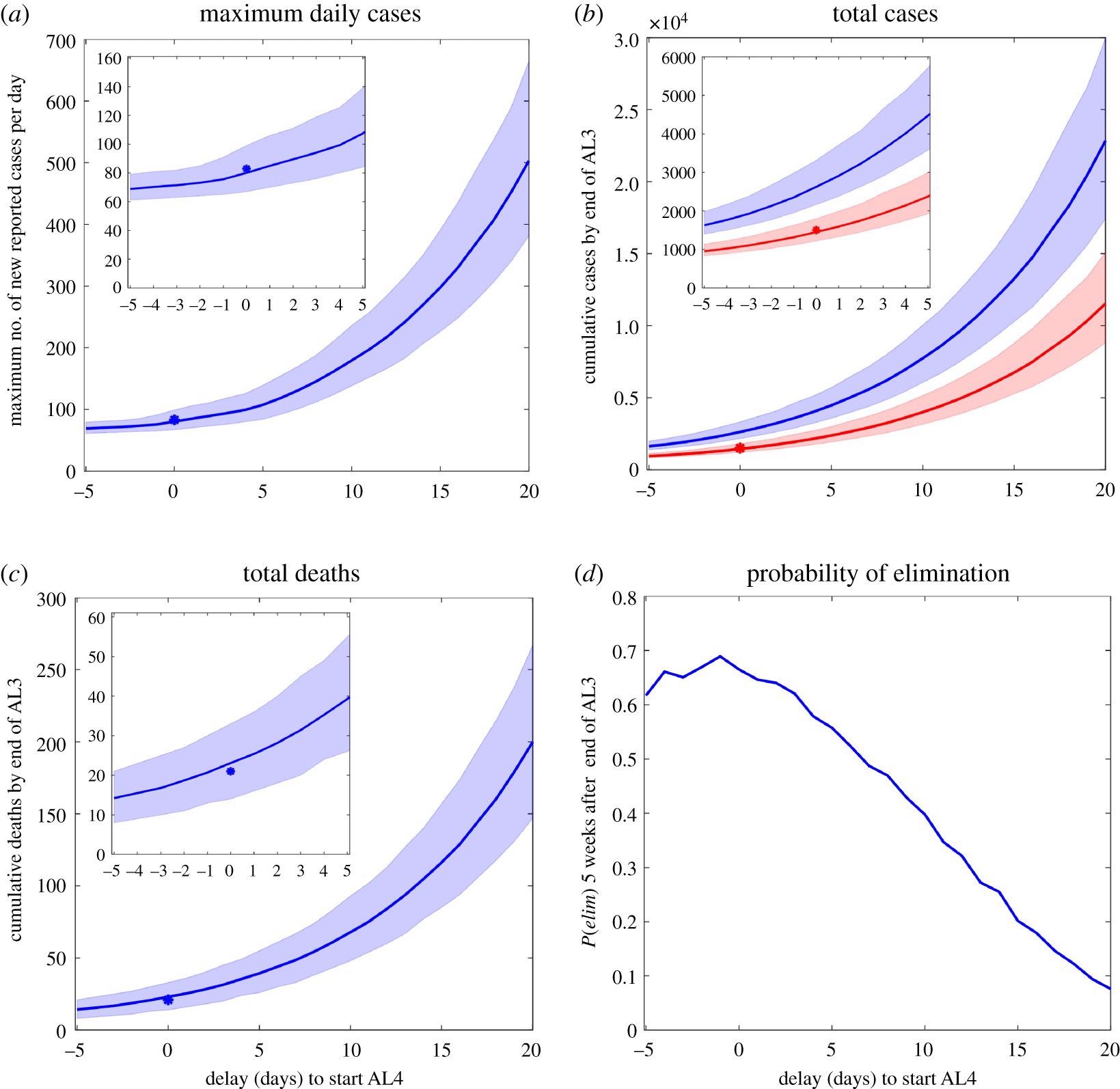 Sensitivity of predicted cases and deaths to varying the delay until start of Alert Level 4, up to a maximum delay of 20 days. A negative delay of 5 days represents starting AL4 5 days early (20 March 2020). Border restrictions and closure were implemented on the same dates as actually occurred. (a) Maximum number of new reported cases per day predicted by the model (blue line) and actual maximum number of daily reported cases (asterisk). (b) Cumulative number of infected individuals (both clinical and sub-clinical) (blue line) and reported cases (red line) predicted by the model and actual number of reported cases (red asterisk). (c) Cumulative number of deaths predicted by the model (blue line) and actual number (blue asterisk). (d) Probability of elimination, P(elim), five weeks after the end of AL3. Shaded regions indicate the interval range in which 90% of simulation results are contained. Note, y-axis scale differs between figures. Insets show close-ups of results for delays from –5 to 5 days.
Sensitivity of predicted cases and deaths to varying the delay until start of Alert Level 4, up to a maximum delay of 20 days. A negative delay of 5 days represents starting AL4 5 days early (20 March 2020). Border restrictions and closure were implemented on the same dates as actually occurred. (a) Maximum number of new reported cases per day predicted by the model (blue line) and actual maximum number of daily reported cases (asterisk). (b) Cumulative number of infected individuals (both clinical and sub-clinical) (blue line) and reported cases (red line) predicted by the model and actual number of reported cases (red asterisk). (c) Cumulative number of deaths predicted by the model (blue line) and actual number (blue asterisk). (d) Probability of elimination, P(elim), five weeks after the end of AL3. Shaded regions indicate the interval range in which 90% of simulation results are contained. Note, y-axis scale differs between figures. Insets show close-ups of results for delays from –5 to 5 days.
In scenario 4, border closure was delayed by five days to all, except the returning citizens. The key measures were only slightly worse compared with scenario 0. However, a delayed border closure greatly impacted the probability of elimination five weeks after AL3 restrictions were relaxed, which was only 55%, compared to 66% in scenario 0.
In scenario 5a, both the border restrictions and the AL4 were implemented five days earlier. The outcomes were similar to those predicted in scenario 1 (where only AL4 started early), reaffirming that they are more sensitive to changes in the timing of AL4 than to the timing of the border restrictions. In scenario 5b, both border closure and AL4 were delayed by five days. The results suggested that the impact of AL4 timing is higher than the impact of border closure timings in containing transmissions.
In scenario 6, border restrictions and border closure were implemented without implementing AL4/3. The results of this scenario demonstrated that border measures alone would have been inadequate to prevent an outbreak and those stringent AL4/3 restrictions were necessary for the elimination of widespread community transmission.
Overall, the results of the study point to two critical observations. First, the timing of AL4 strongly drives reductions in daily new cases as against the timings of border measures. This justifies using a study model designed to use the AL4 effect to reduce Reff values to as low as 0.35 for all domestic and international arrivals. Second, of all the scenarios, the one in which AL4 was earlier by five days resulted in the highest reduction in cases and deaths as indicated by ~500 fewer cases in total and ten fewer deaths.
Future directions
The study's results effectively demonstrate that the early intervention was critical to the successful control of New Zealand's March–April 2020 COVID-19 outbreak relative to alternative scenarios.
This one-of-its-kind early intervention strategy could help guide future response strategies. Hence, the inferences of this study should be factored in when designing models for future disease outbreaks besides updating epidemiological parameters to implement improved response plans and policies. This is further supported by the results showing that the degree of compliance with AL restrictions changes in the future will result in different Reff values.
Further, the social dynamics affecting transmission and the effectiveness of interventions should be explored. That would make it easier to ascertain the impact of people wearing masks in public spaces or avoiding travel if a suspected new outbreak is reported.