Coronavirus disease 2019 (COVID-19) has spread to nearly every country in the world and is responsible for over 5 million deaths. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the organism that causes the disease, infects epithelial tissue in the lungs, later destroying endothelial cells. This can cause massive inflammatory and immune reactions, and infected individuals can suffer from very varied symptoms, from a mild cough to multiple organ failure.
The extensive inflammatory response that is characteristic of more severe disease is thought to increase the production of reactive oxidative species that can cause even more harm to the body. Serum-free thiols are known to reflect the activity of reactive oxygen species in the body, and a group of researchers from the University of Groningen have been examining the difference in these thiols in COVID-19 patients.
Study: Mild Coronavirus Disease 2019 (COVID-19) Is Marked by Systemic Oxidative Stress: A Pilot Study. Image Credit: SWKStock/Shutterstock.com
The study
The scientists examined data from patients in the Netherlands who had a confirmed diagnosis of COVID-19 using a positive PCR test. No patients were vaccinated. Serum samples were gathered from these, and a roughly equal population of healthy controls. Demographic and clinical characteristics were gathered, including age, BMI, medical history, smoking status, gender, and comorbidities.
The serum was tested for serum-free thiol as well as hemoglobin, C-reactive protein (CRP), white blood cell counts, albumin, and creatine. Hemoglobin, white blood cells, and platelets were measured using an automated hematology analyzer, albumin and CRP were measured with turbidimetry, and estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula. The basic characteristics were presented as means +/- standard deviation, and medians in case of non-normal distributions.
Shapiro-Wilk normality tests, histograms, and Q-Q plots were used to assess normality. Mann-Whitney U-tests and independent sample t-tests were used to assess differences between groups of continuous samples, and nominal variables were compared using chi-square tests or Fisher’s exact tests. Paired t-tests were used for within-group comparisons. Univariable and multivariable linear regression analyses were used to identify parameters associated with serum-free thiol concentrations.
The researchers examined 29 mild, non-hospitalized COVID-19 patients and 30 healthy controls. There were no significant differences in age, gender, or body mass index between the groups. Comorbidities such as smoking history, hypertension, diabetes, and pulmonary disease were also equal between groups. Differences were observed in concentrations of CRP (increased in COVID-19 patients) and concentrations of WBC (decreased), but this is expected. COVID-19 subjects showed a wide range of symptoms, including asymptomatic patients and several who suffered from ‘long COVID’. Seven hospitalized patients were also examined.
The researchers found that serum-free thiol concentrations were significantly reduced in patients with mild COVID-19, and albumin-adjusted serum concentrations of free thiols showed a similar trend with lower concentrations in COVID-19 subjects – although the albumin data was not statistically significant.
The scientists then performed univariable and multivariable linear regression analyses to identify parameters associated with serum-free thiol concentrations. Univariable regression showed that both CRP and albumin concentration were associated with serum-free thiols in COVID-19 patients, while the multivariable regression analysis showed that albumin concentrations were independently associated with serum-free thiol concentrations.
CRP was not associated with albumin. In controls, age and albumin concentrations showed associations with serum-free thiol concentrations. Age and albumin were also associated with each other.
Following this, analyses were performed on the serum-free thiol concentrations at different time points in hospitalized and non-hospitalized COVID-19 patients, to examine any correlation between free thiols and COVID-19 disease severity. While there was no difference between the two groups at baseline, non-hospitalized patients showed significantly lower concentrations of serum-free thiols by day 7, as well as decreased concentrations of hemoglobin and creatinine.
Serum-free thiol concentrations were also evaluated for the ability to differentiate between non-hospitalized patients and controls. The free thiol concentrations differed significantly between these two groups, showing a slightly better discriminative capacity than CRP concentrations. Albumin-adjusted free thiol concentration was also evaluated and found to be effective if less so than free thiols alone. Unfortunately, free thiols were not useful for discriminating between hospitalized and non-hospitalized patients at their baseline.
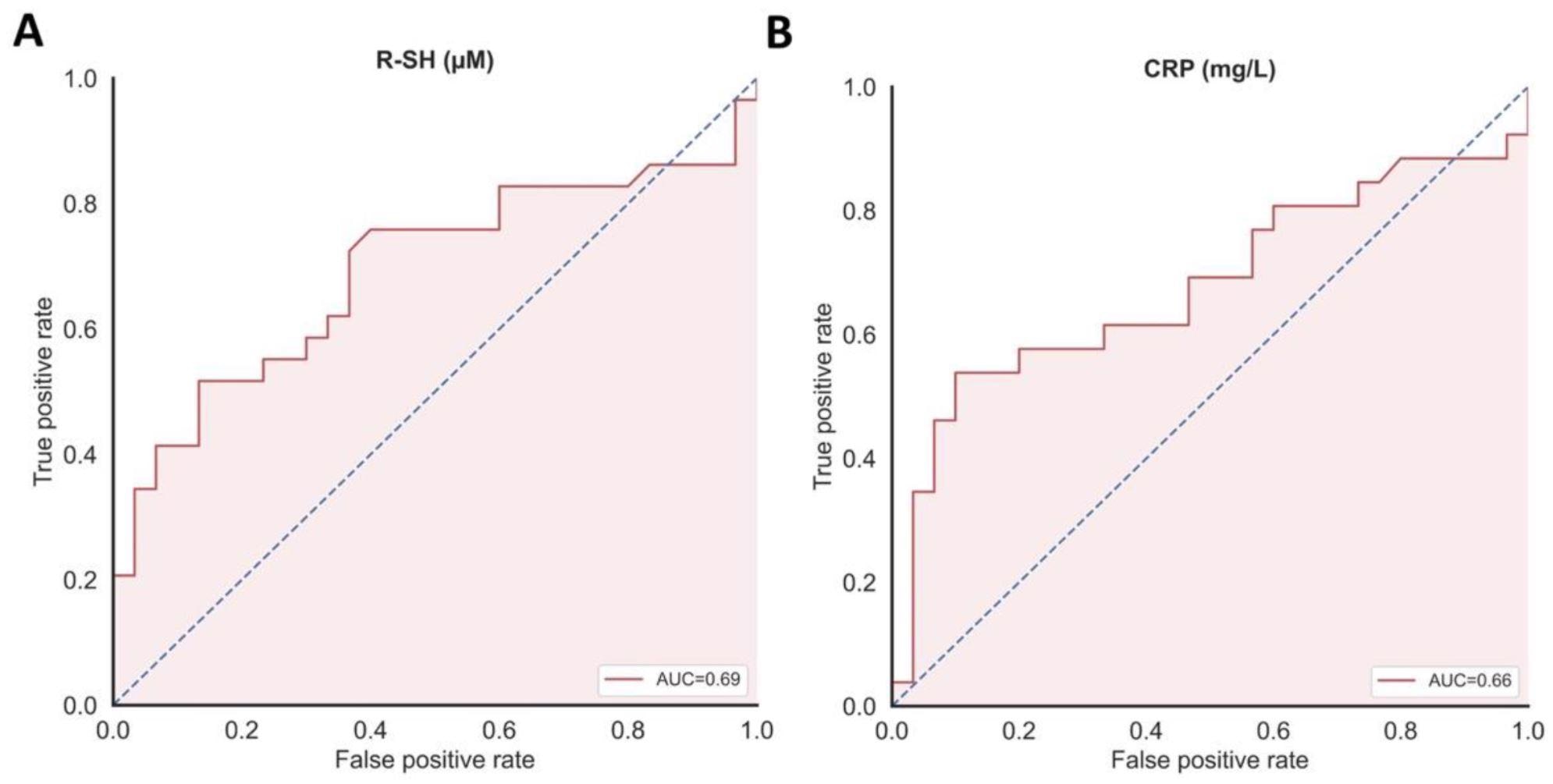
(A) Serum concentrations of free thiols (µM) significantly discriminated between patients with COVID-19 and healthy controls and (B) showing a slightly higher discriminative capacity as compared to CRP concentrations (mg/L).
The conclusion
The authors highlight that their study effectively demonstrates that serum-free thiols are significantly lower in patients with COVID-19 compared to the control group. This is significant evidence for the presence of a redox imbalance in even mild COVID-19 patients. This information could be very valuable for healthcare workers and drug developers.
While unfortunately the presence of serum-free thiols cannot be used as a biomarker for future disease severity at baseline, it could still be used to measure the advancement of the disease.
Journal reference:
-
van Eijk LE, Tami A, Hillebrands J-L, den Dunnen WFA, de Borst MH, van der Voort PHJ, Bulthuis MLC, Veloo ACM, Wold KI, Vincenti González MF, van der Gun BTF, van Goor H, Bourgonje AR. Mild Coronavirus Disease 2019 (COVID-19) Is Marked by Systemic Oxidative Stress: A Pilot Study. Antioxidants. 2021; 10(12):2022. https://doi.org/10.3390/antiox10122022